Podcasts
Clinical
OTC
Practice
Addiction
Allergy
Cancer
Child & teen health
Clinical services
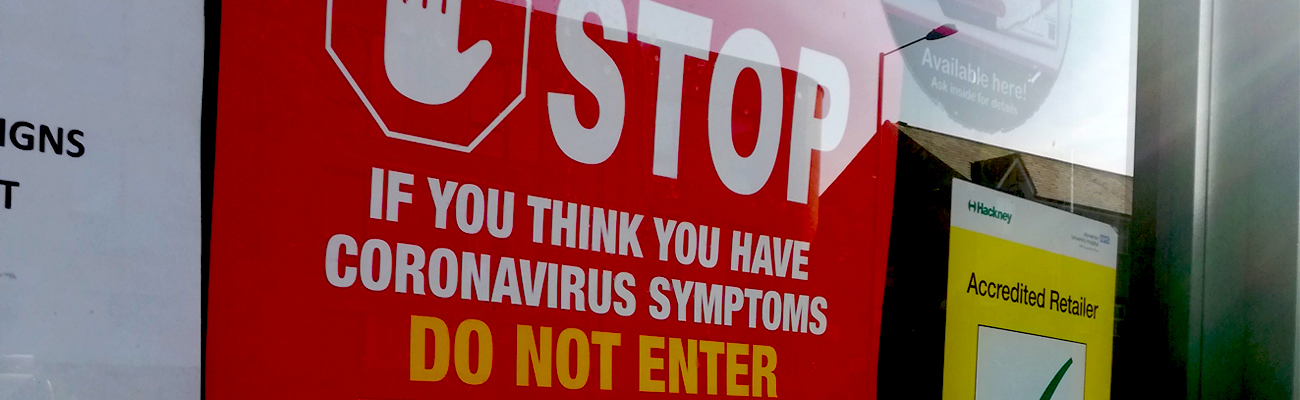
Coronavirus
Cough & cold
Dementia
Diabetes
Digestive health
Eyes & ears
Finance
First aid
Flu
Footcare
Healthy living
Heart health
Incontinence
Infection
Joint health
Leadership
Legal
Lung health
Management
Marketing
Men's health
Mental health
Nervous system
Nutrition
Older people
Oral health
Pain relief
Patient safety
Pet health
Pregnancy & baby
Prescribing
Property
Screening
Services
Sexual health
Skin conditions
Sleep
Smoking
Sore throat
Supplements
Technology
Travel health
Vaccines
Women's health
Popular Searches
Log in
Sign up
Recommended Help
Search by Keyword
Most popular questions
Is registration FREE?
Yes, registration is absolutely FREE
How long does it take to register an account?
It takes less than a minute to create your secure account – you just need to tell us a few details about yourself and create a password.
I can’t remember my password
Please click on the “Forgot my password” link in the login form and follow the instructions.
I can’t remember the email address I registered my account with
Please email info@pharmacy-network.co.uk so we can check for you.
What learning content do you have?
Pharmacy Magazine contains a library of high-quality educational e-learning modules, videos and articles to support your ongoing learning.
Is the learning suitable for all pharmacy team members?
Yes, we have content suitable for all abilities, with topics covering business management, clinical, practice and OTC. Our aim is to help you keep up to date and develop your skills and knowledge to positively influence patient outcomes and customer experiences.
Can I access the library on my mobile?
Yes, you can access all learning at work or at home on any mobile, PC or tablet device
What’s the best way for me to find relevant content for my role?
There are three ways you can find relevant content. Firstly, the homepage will display suggestions for you. If you are logged in, we can tailor the content to your particular job role and topics of interest, as well as making it easy for you to see what’s trending. Secondly, you can use the “search” function at the top of the website. Finally, you can click on “explore” in the main menu and browse topics of interest to you.
How long do modules take?
We have a range of modules and videos ranging from 2 minutes up to 15 minutes. There is something for everyone, even if you are short on time.
Can I save content for later?
Yes. If you see a piece of learning you would like to take, but haven’t got time right now, you can “Bookmark” it for later. Please note you need to have a registered account and be logged in to access this feature.
Can I record my learning outcomes?
Yes, logged in members can record their learning outcomes on any piece of content and save them in their learning log. Pharmacists and technicians can do this using recording templates in line with GPhC requirements.
How do I get a learning log?
You have to register an account on Pharmacy Magazine and login to access your personal, secure learning log.
What does my learning log do?
It documents all the learning you have recorded, including completed learning, learning in progress and bookmarked learning you have saved to do later.
If I’m a pharmacist or pharmacy technician, can the log help me fulfil the GPhC’s revalidation requirements?
Yes, pharmacists and pharmacy technicians also have the ability to record and add their own revalidation entries to their learning log in line with GPhC requirements.
If I’m a member of more than one website on The Pharmacy Magazine, can I access all my learning in my learning log even if I’ve recorded it on different websites?
Yes, if you record learning on more than one website, it will be displayed in your learning log which is shared across all the accounts you have registered with The Pharmacy Magazine.
How do I view/print a certificate of my learning?
Certificates are available at the end of every module, after the assessment questions. They are also accessible via the learning log.
How do I change my personal details, email address and password?
Login and click on “Settings” in your member menu and click on the relevant links to change any of your details. All saved changes take immediate effect.
If I leave the industry and want to delete my account, can I do so?
Yes absolutely. You are able to delete your account at any time but please be aware that by doing so you will also delete any historical learning records you have in your learning log.
If I have a query or I’m stuck, how can I get help?
You will need to have registered an account to get help. Logged in members can click on the “Helpdesk” link in their Settings and submit a Helpdesk ticket. We endeavour to respond to new Helpdesk tickets within 24 hours during office hours (9pm to 5pm Mon to Fri)
How can I check on your Terms of Service, Privacy Policy and Cookie Policy?
You can click on the relevant links in the footer of the website. If there are any proposed changes to any of our Policies, we will email registered members in advance.
Is Pharmacy Magazine GDPR compliant?
Yes we are and we take your privacy and the security of your data extremely seriously. Please read the Privacy Policy for further details. Logged in members can click on the “My data” link in “Settings” to download a copy of all the personal data we currently hold on you.
Who is the company that owns and operates Pharmacy Magazine?
Communications International Group Limited (CIG), the largest, most experienced publisher in the UK pharmacy sector. CIG is the UK’s leading provider of sector-specific news and training, publishing 15 healthcare and beauty titles including Pharmacy Magazine, Training Matters, P3Pharmacy, Independent Community Pharmacist and Beauty Magazine. Over the years the company has built an enviable reputation in pharmacy, journalism, education, training, regulatory, awards and conferences, that today amounts to more than 350 years of healthcare industry experience.
How do I sign out?
Click on the Sign Out link that can be found at the top of the website, in you member menu.