Bladder weakness: Tapping into a growing market
In Clinical
Follow this topic
Bookmark
Record learning outcomes
What does your pharmacy offer those customers who need help with bladder weakness? If the answer is 'not much', you could be missing out on a market that is rapidly becoming mainstream...

Learning objectives
After reading this feature you should be able to:
- Identify the common causes of urinary incontinence and bladder weakness
- Understand the debilitating impact incontinence has on sufferers
- Provide discreet advice to help improve the quality of life of bladder weakness sufferers.
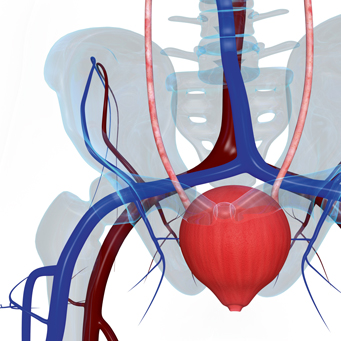
To work properly, the urinary system needs the brain, muscles and nervous system to all function together, but there are many factors that can interfere with this process. Urinary incontinence affects people of all ages. Other than older people, those most at risk are women after pregnancy or around the menopause and men after prostate cancer treatment.
€Abdominal pressure during pregnancy and a reduction in the quantity of oestrogen [produced] during the menopause can weaken the pelvic floor muscles that keep the urethra closed,€ says Donna Wilson, TENA training and brand manager. €When these crucial muscles lose their elasticity, everyday activities such as laughing, coughing and exercising can cause bladder weakness.€
The cause and type of incontinence can often be identified after a consultation with a GP, who will ask about the symptoms and undertake a pelvic examination (in women) or rectal examination (in men). Patients may be asked to keep a diary, recording how much they drink each day and how much and how often they urinate.
It is important that urinary incontinence is diagnosed and treated as soon as possible, as the symptoms can become worse over time. It is also important that customers seek help if they experience pain with urination.
There are several different forms of urinary incontinence:
- Stress incontinence causes urine leakage at times of pressure, such as sneezing, coughing, bending or lifting heavy weights. Often caused by weak pelvic floor muscles, the amount of urine passed is small, although this increases if the bladder is full
- Urge incontinence is a leakage that is so sudden that it is impossible to get to a toilet in time. The need to pass urine can be triggered by a change of position or even the sound of running water. Urge incontinence is often associated with an overactive bladder (when the bladder muscles are more active than usual), which can cause a frequent urge to urinate, especially at night
- Mixed urinary incontinence is a mixture of the stress and urge varieties
- Overflow incontinence (chronic urinary retention) is when someone is unable to fully empty his/her bladder, which causes leakage. The bladder may swell up and never feels completely empty. This may be caused by an obstruction or blockage, such as an enlarged prostate, constipation or bladder stones
- Total incontinence is when the bladder can't store any urine at all, leading to frequent leakage. This is usually caused by a problem with the bladder from birth, a spinal injury or a bladder fistula.
The normal number of times to pass urine each day varies between six and eight and one per night, says Marta De Oliveira, women's health physiotherapist at BMI London Independent Hospital. €If a person experiences involuntary leakages of urine with exertion, increased frequency during the day and night, and urgency to urinate with or without leaks, it is important to seek help.€
Who is at risk?
Family history and ageing both increase the likelihood of developing urinary incontinence. However, incontinence is not an inevitable part of ageing and should always be investigated. Stress and urge incontinence are the commonest forms of incontinence seen in primary care.
€Bladder overactivity develops either out of the blue or due to a blockage of the bladder outlet; for example, from enlargement of the prostate or tightness of the [urethra],€ says Maya Harris, consultant urological surgeon at Spire Parkway Hospital in Solihull.
€Stress incontinence is due to weakness of the bladder outlet due to labour or after removal of the prostate gland. Infection and constipation are frequent causes of incontinence and are well worth checking for as they are easily treatable. If bladder symptoms develop suddenly and quickly, this can be a sign of a serious underlying condition, such as pelvic swelling.€
Common risk factors include chronic constipation, obesity, urinary tract infections, pelvic organ prolapse, hormonal changes in women (e.g. oestrogen deficiency at the menopause) and prostate problems (or treatment for prostate problems) in men.
Some medication (e.g. antidepressants, diuretics, hormone replacement therapy and sedatives) can affect the storage, passing or quantity of urine. Neurological problems, such as multiple sclerosis, may also be responsible for incontinence.
Management approaches
There are various treatments for urinary incontinence, depending on the underlying cause and the severity of the symptoms. The first step is to try treatments that don't involve medication or surgery.
According to Maya Harris, many patients delay seeking medical help unnecessarily. €Patients should come forward as soon as bladder weakness and incontinence starts affecting their everyday life,€ she says. €In my experience, many patients still encounter social stigma due to bladder problems. For example, they ask me to provide them with special letters advising about their condition, as the general public is reluctant to understand that they require the urgent use of a toilet €“ for example, in a shop.€
General advice for people with any form of urinary incontinence includes losing weight (if customers are overweight or obese) and cutting down on caffeine and alcohol, as these can irritate the bladder. Caffeine also increases the amount of urine produced. Pharmacists can advise on a suitable fluid intake €“ drinking too much or too little can exacerbate the problem.
Many people who experience increased urination at night limit their fluid intake in the early evening but they should make sure they drink plenty of fluids during the day to compensate.
If customers have urge incontinence, they may be referred for bladder training. This involves learning how to wait longer between feeling the need to urinate and passing urine. The course often lasts for six weeks or more and may be combined with pelvic floor muscle training.
Pelvic floor muscles are the muscles that control the flow of urine during urination. If they are weak or damaged, for example during pregnancy or childbirth or after prostate surgery, this can cause urine leakage. Pelvic floor exercises involve contracting the pelvic floor muscles at least three times a day, for at least three months. A GP can refer a customer to a specialist continence physiotherapist for an individual exercise programme.
€The best way to activate the pelvic floor muscles is to tighten around the front and back passage at the same time as if trying not to pass wind and urine,€ says Marta De Oliveira. €It is important to avoid breath holding as well as squeezing the muscles of the buttocks and thighs when doing these exercises. Some people find it really hard to activate or fully relax these muscles or feel pain when doing the exercises.
€In these cases, the gold standard is to have a pelvic floor assessment with a specialist physiotherapist. As with other types of muscle training, it is more about using the correct technique, because if the exercises are not done well, they cause more problems or will not help at all.€
Rizwan Hamid, consultant urological surgeon at the Princess Grace Hospital in London (part of HCA Healthcare UK), agrees that the best results occur when people carry out the exercises under the supervision of a trained nurse or physiotherapist.
€This is because patients need to understand how to undertake the exercises properly. For example, knowing what muscles they're using, what the frequency should be and how best to incorporate these exercises into their daily routine. For those looking to try the exercises at home, there are a number of leaflets available, along with training videos so people can see if they are doing them correctly.€
Medication, such as antimuscarinics for an overactive bladder, may be recommended for customers who are still unable to manage their symptoms after lifestyle advice, bladder retraining and pelvic floor exercises. Surgery is available for stress incontinence if other treatments are unsuccessful, to reduce pressure on the bladder or strengthen the muscles controlling urination.
Key facts
- Many patients delay seeking medical help unnecessarily for bladder weakness problems
- The normal number of times to pass urine each day varies between six and eight and once per night
- Customers may be reluctant to start a conversation about bladder weakness at the medicines counter, so pharmacy staff have to be prepared to take the initiative
Pharmacy advice
Customers expect the following from the bladder weakness category in pharmacy, says Cathy Crossthwaite, Numark retail marketing co-ordinator:
- A product range to suit multiple needs in a variety of fits
- The category positioned away from the hustle and bustle of the pharmacy with the option to purchase discreetly
- The choice to read or take away supporting information
- The opportunity for a private consultation to discuss potentialproduct choices and management tips.
Pharmacies can stock various products to help incontinence sufferers deal with urine leakage, such as pads and pants, and sheaths for men. Customers can also buy incontinence bedding (e.g. washable bed pads), skincare products to prevent rashes and soreness, and products to help them with pelvic floor exercises. However, sufferers may well be reluctant to start a conversation at the counter, so pharmacy staff have to be prepared €“ with great sensitivity €“ to take the initiative.
Pharmacy teams are ideally placed to provide advice on selfhelp measures and lifestyle changes, not only verbally but also with leaflets, POS materials and window displays. They can also signpost customers to useful websites, such as those run by the manufacturers of bladder weakness products and NHS Choices.
By providing self-serve information at the fixture, customers can pick and choose when they interact with a member of the pharmacy team, says Cathy Crossthwaite. When speaking to customers, teams must interact with discretion and sensitivity, she emphasises.
€It may be beneficial to offer 'point-to cards' for discreet product choice. The taboo of bladder weakness is slowly lifting with the ongoing work that manufacturers are carrying out to promote products and desensitise consumers, making the condition more talked about and better understood.€
€Pharmacies have a consultation room or quiet area, which means confidential support can be readily available for such a difficult topic,€ says Thorrun Govind, community pharmacist at Sykes Chemist in Bolton.
€Products should be placed in a quiet part of the pharmacy where customers can discretely walk around and feel more comfortable. The fixture can be very confusing, which is why people often use sanitary towels instead. Pharmacists and pharmacy staff are well placed to discuss whether customers are using the right products. It is important to advise that specific bladder products are more absorbent, feel more secure and lock in the odour and moisture.€

New technology has made disposables even more effective, says Sadik Al Hassan, a pharmacist at Well, who notes that Age UK now has its own range of incontinence products that are gaining in popularity.
€There are also trends that indicate new technology could see the return of more stylish washable incontinence products like New Zealand's Confitex,€ he says. €These new high-tech fabric products combat one continuing problem with disposables €“ they look like conventional underwear.€
Certainly, innovation in this category has been focused onenhancing style and fit so that users feel safe and comfortable when wearing these products. TENA's latest pants launch sees different design features for both men and women. While TENA Lady Pants Plus are designed with the female anatomy in mind and are finished in a soft peach colour €to give an air of femininity that wouldn't look out of place in an underwear drawer€, TENA Men Active Fit pants have a boxer-like design and a navy blue finish, says Donna Wilson.
Mix and match
Shelagh Clark, team leader pharmacy UK at P&G, says pharmacy staff can identify the correct product for each customer by establishing the level and cause of incontinence. €For stress incontinence caused by coughs or sneezing, liners or pads should be enough,€ she says. €For urge incontinence, customers should consider pads or pants. You should recommend pads or pants for mixed incontinence as well.
€Choose the right level of absorbency by finding out the amount of urine loss. If it is a small amount causing moisture, suggest using liners or pads. For leaks causing wetness, recommend moving to higher absorbency pads. With significant urine loss, a customer might want to consider using specialised pants.
€Find out about the situation in which the product is used. If the person is in a secure environment, such as at home, a lower absorbency product might be enough. If he or she is participating in outdoor sports with the nearest toilet some distance away, they might require a higher absorbency [product].€
A display offering advice on bladder weakness products, how to stay healthy and when to see the GP is great for starting conversations with patients on this difficult subject, says Sadik Al Hassan, €but even without a health promotion area, you could still have a focus on bladder weakness in your pharmacy. Make sure that every member of your team feels confident talking about the topic €“ role play and team huddles could help your staff have greater knowledge about all aspects of bladder weakness€.
Benign prostatic hyperplasia
Problems associated with the prostate gland are one of the most likely causes of urine leakage in men, says TENA's Donna Wilson.
Benign prostatic hyperplasia (BPH) is the enlarging of the prostate gland. While it is common for the prostate to increase in size as a man ages, causing pressure on the urethra, in more severe cases this can lead to overflow urinary incontinence (a complete emptying of the bladder).
In some cases nerves and muscles are damaged during surgery, which can cause a more permanent problem. These muscles keep the bladder closed, so damaging them can lead to symptoms similar to those experienced by women.
Pelvic floor aids
A number of pelvic floor aids are available, which may help customers do the exercises more effectively. Vaginal cones are small weights inserted into the vagina like a tampon and held in place using the pelvic floor muscles. Some women find these uncomfortable or unpleasant to use, but the cones may help with stress or mixed urinary incontinence. As a customer's pelvic floor becomes stronger, they can add more weights and increase the time they keep the cone in place.
Biofeedback devices monitor how well people are doing their pelvic floor exercises. One exerciser provides a visual way of seeing whether the pelvic floor exercises are being done properly €“ when the pelvic floor muscles contract correctly, the indicator moves downwards. There are also more complicated electrical biofeedback machines.
€A number of studies have demonstrated that vaginal cones and biofeedback exerciser aids are powerful tools in training pelvic floor muscles,€ says Marta De Oliveira. €For some people, using these devices helps to improve compliance to treatment or training and improves motivation levels. They also provide objective outcome measures.
€It is very important to say that none of these devices should be used without seeing a specialist physiotherapist beforehand for a thorough assessment and prescription of a supervised and individualised pelvic floor muscles exercise programme.€
The British Association of Urological Surgeons provides information on pelvic floor exercises for men and women at baus.org.uk.
When to refer...
As with any condition there are things to look out for that necessitate a referral:
- Signs of infection
- If there is blood
- If there is pain around the kidneys
- The condition is worsening.
Advising on bladder weakness
The onset of bladder weakness can depend on many influences. Because of this, it is important for pharmacy teams to understand the underlying cause in order to offer the most effective advice, says Donna Wilson, TENA training and brand manager. €It is vital for pharmacy staff to try and understand the anxiety a person may be feeling when opening up about their concerns,€ she says.
Recent research from TENA has revealed that one in seven women and one in eight men will visit their local pharmacy rather than their GP for advice about bladder weakness, making it one of the fastest growing OTC categories in pharmacy.
With this in mind, a full range of bladder weakness products should be displayed in pharmacies, ranging from a low level of support to the heavier incontinence pads. Customers should be able to browse the range and ask trained advisers questions, removing the need for lengthy GP waiting times.
€Pharmacies are trusted environments, and as such, customers feel it is a safer environment to purchase bladder weakness products, especially if seeking additional advice,€ says Wilson. €This is especially advantageous as it allows pharmacists and their teams to build a rapport with the local community, understand the particular needs of bladder weakness sufferers, and how to then respond with meaningful advice that will enable them to live their lives to the full.€
Fix your fixture
A common error within pharmacy is to allocate too much space to feminine hygiene, which is more likely to be a distress purchase category, whereas bladder weakness should be the focus for the fixture and act as the destination segment for customers, says Cathy Crossthwaite, Numark retail marketing co-ordinator.
If you break the feminine hygiene and bladder weakness sectors down into a number of sub-categories, it is clear to see that bladder weakness dominates, with a 73 per cent share of space, she says.
€There are arguments that bladder weakness and feminine hygiene should be separated, but this would depend primarily on the space available in the pharmacy. The adjacencies of the categories go hand in hand and customers have come to expect the two to sit together. The problem, which often occurs, is that pharmacy tends to dedicate too much space to feminine hygiene products, when the expertise and confidence to deliver it lies in bladder weakness.
€Through combining the feminine hygiene and bladder weakness categories into a single bay, it is more likely that a wide range of customers will visit €“ from young teenagers who are just starting their cycle to elderly women and men struggling with bladder weakness. The product range stocked should suit each of these customers and pharmacy teams should be armed with the advice and guidance to help them.
€To help customers choose the right products, ensure there is a clear distinction between feminine hygiene and bladder weakness products. Use signage and shelf inserts to help customers understand where the categories are separated.€
Pharmacy teams must interact with discretion and sensitivity
