Scratching the surface
In Clinical
Follow this topic
Bookmark
Record learning outcomes
With an estimated 8 million people currently living with skin disease1 and a recent report suggesting major failings in NHS dermatology services, there is a need for greater pharmacy involvement in managing skin conditions in primary care.
Learning objectives
After reading this feature you should be able to:
- Recognise the warning signs and symptoms suggestive of potential skin cancer
- Appreciate the psychological impact of dermatological disorders
- Discuss the research presented at the recent annual meeting of the British Association of Dermatologists.
A recent report carried out by the King's Fund has uncovered major failings in NHS dermatology services.2 The report revealed significant shortfalls in several key areas in the management of chronic skin diseases including:
- Lack of adequate staffing
- Poor training
- Inconsistent quality in diagnosis and treatment
- Large variations in access to specialist care.
According to the report, an estimated two-thirds of patients with skin problems opt to manage their condition through self-care €“ although some estimates suggest this figure may actually be as high as 86 per cent.2
Seventeen per cent of all current OTC sales are for skincare products, putting skincare on a par with cough/cold remedies and second only to pain relief as the largest overall OTC pharmacy category.3 The wide range of skin-specific medications now available from pharmacies provides the scope for effective self-care of a variety of different dermatological conditions.
As the King's Fund report points out: €The opportunity to support self-care is significant, reflected by spend on OTC sales €“ people spent £413m on OTC skin treatments in the UK in 2007. This may be due to high levels of willingness to pay for effective treatments for acne, atopic eczema and psoriasis.€
Evidence also indicates that skin conditions account for up to a quarter of all symptom-based requests for advice in community pharmacy.3 All of this combines to highlight a potentially important role for community pharmacists in helping to facilitate effective self-care for patients with skin problems.
Supporting self-care
Psoriasis
 Psoriasis affects around 2 per cent of the UK population, manifesting as characteristic pink or red skin lesions covered with silvery-white scales.4 One of the key areas for pharmacy support in the self-care of this skin condition is in maximising the benefits from OTC and/or prescribed psoriasis therapies. A range of emollients are available OTC for the relief of psoriasis symptoms.
Psoriasis affects around 2 per cent of the UK population, manifesting as characteristic pink or red skin lesions covered with silvery-white scales.4 One of the key areas for pharmacy support in the self-care of this skin condition is in maximising the benefits from OTC and/or prescribed psoriasis therapies. A range of emollients are available OTC for the relief of psoriasis symptoms.
The key to maximising their treatment benefit is to use liberally and often. Emollients should be applied about 30 minutes before treating with specific prescribed psoriasis topicals as they can help to promote penetration of the active agent into the skin. Emollients should also be used as a soap substitute whenever bathing or washing but customers should be advised to take additional care with salicylic acid-containing emollients as these may irritate the surrounding healthy skin.
Several coal tar-containing products for psoriasis are also available, including ointments, creams and shampoos. Coal tar can irritate or redden the skin, so is not suitable for treating more inflammatory forms of psoriasis. It can also stain clothing, bed linen and hair so must be applied carefully only to the affected areas of skin.
Customers using coal tarbased products should be warned that sensitivity to sunlight will be increased and tar will remain active on the skin for at least 24 hours, so a sunscreen should be used and sun exposure carefully controlled. With all topical therapies, continuous treatment of psoriasis, even when symptoms appear to improve, is important to prevent further skin flare-ups. When it comes to more general self-care measures, patients with active psoriasis should be advised to reduce their alcohol consumption and cut down (or ideally quit) smoking €“ both of which can exacerbate symptoms.
Adopting a healthy lifestyle, through positive dietary changes and increased physical activity, is also recommended given the recently confirmed link between psoriasis and a raised risk of cardiovascular (CV) disease, diabetes and obesity. Stress management may be beneficial for patients.
Pharmacists should additionally be aware of the commonly-used medications that can aggravate or provoke psoriasis including lithium, some antimalarials, beta-blockers, NSAIDs and ACE inhibitors. Detecting this type of adverse reaction is complicated by the fact that drug-induced skin symptoms of psoriasis may not manifest themselves until the medication has been taken for several weeks or even months.5
Eczema
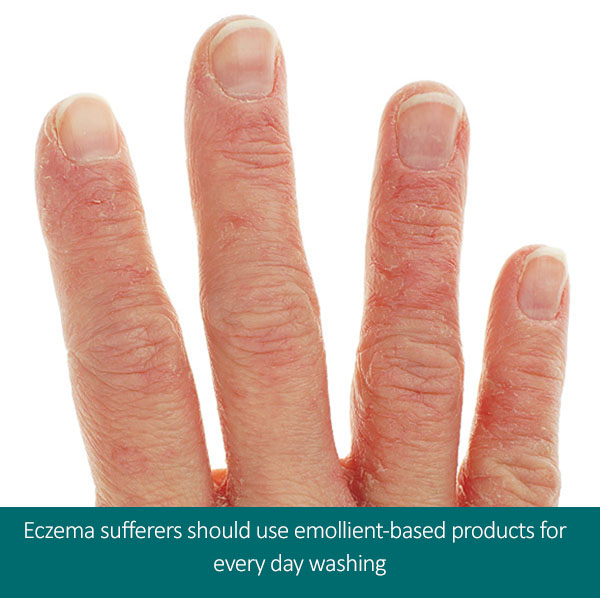 Eczema is a common skin condition where good pharmacy-led self-care can have a significant positive impact on patient outcomes. Important advice for sufferers should focus on the following key counselling points:
Eczema is a common skin condition where good pharmacy-led self-care can have a significant positive impact on patient outcomes. Important advice for sufferers should focus on the following key counselling points:
- Avoid habitual scratching that can damage the skin €“ keep nails short, keep skin covered with light clothing and try gentle rubbing of the skin with the fingers as an alternative to more vigorous scratching
- Take steps to identify and avoid specific allergic eczema triggers, which may include certain fabrics, heat, the use of particular soaps or detergents, or dietary components such as eggs or cows' milk
- Use emollients several times daily (or more often if skin is very dry), even when not experiencing symptoms.
Correct emollient use is the cornerstone of effective treatment of eczema. Important practical points for pharmacists to emphasise are to use a large amount of emollient, apply after bathing to the whole body, and smooth into the skin in the direction of hair growth. Using a spoon or pump to dispense emollient is preferable to placing fingers directly into the pot, as this increases the risk of infection.
Bacterial infection (most commonly with Staph aureus) will exacerbate eczema symptoms and requires antibiotic treatment.5 NICE suggests that eczema sufferers use emollient-based products as an alternative to soaps and detergents for everyday washing, bathing and moisturising. Emollients can be used safely in conjunction with other stronger eczema treatments, such as topical corticosteroids.
Acne
Most cases of mild acne can be treated successfully with benzoyl peroxide-containing creams or gels. Benzoyl peroxide is a mild antiseptic, which acts against the acne-causing bacterium, Propionibacterium acnes, and also possesses anti-inflammatory properties. Customers should be advised to apply benzoyl peroxide once or twice a day, 20 minutes after washing acne-affected areas of the face. Some mild irritation, redness or peeling of the skin is common and sun-sensitivity is also increased.
As the name suggests, benzoyl peroxide has a bleaching effect so contact with hair or skin should be avoided. In addition to optimising use of OTC acne products, pharmacists can also offer advice to help reduce acne symptoms and/or limit future skin outbreaks.
Despite the temptation to wash more regularly, acne sufferers should limit washing of the affected area to no more than twice daily using a mild soap or cleanser and lukewarm water. Squeezing spots can aggravate the bacterial infection and even promote permanent scarring, so should be discouraged. Pharmacy staff can also suggest the following self-care tips:
- Use non-comedogenic, water-based cosmetics
- Always remove make-up before bed
- Use a fragrance-free, water-based emollient if dry skin is a problem
- Wash hair regularly to prevent the build-up of grease
- Avoid contact between the hair and the face wherever possible (e.g. cut or clip back a long fringe).
For more severe cases of acne with widespread pustules and papules that are unresponsive to OTC products, customers should be referred to their GP for treatment advice on some of the stronger antibiotic and hormonal therapies available on prescription.
Conference round-up
Dr Christine Clark reports from the recent British Association of Dermatologists (BAD) annual meeting
Trials focus on filaggrin gene
Two important trials are looking at the role of the filaggrin gene (FLG) in the management of atopic eczema, delegates at the BAD conference were told. The Barrier Enhancement for Eczema Prevention (BEEP) and Clothing for the relief of Eczema Symptoms (CLOTHES) trials will separate participants according to FLG status in order to see whether this important barrier protein influences their responses. BEEP is looking at whether the regular use of emollients in the first year
of life can prevent or delay the onset of eczema in high-risk children.
The basic premise is that skin barrier dysfunction makes the skin more vulnerable to damage due to environmental factors and this eventually leads to the development of eczema. The BEEP study is funded by the National Institute for Health Research and will recruit 1,300 participants. CLOTHES is looking at the impact of therapeutic (prescribable) silk clothing on 300 children with moderate to severe eczema (in the UK) over a six-month period.
Although some silk clothing is prescribable, studies to-date have been too small and too short to allow firm conclusions about effectiveness to be drawn. Absence of filaggrin leads to a poorly formed stratum corneum that is prone to excessive water loss and therefore dryness.
Loss-of-function mutations of FLG occur in up to 10 per cent of people and are strongly associated with ichthyosis vulgaris. They also increase the risk of developing atopic eczema, asthma and peanut allergy.
Daylight-activated photodynamic therapy for AKs
Daylight-activated photodynamic therapy (dPDT) for actinic keratoses (AKs) causes less pain than conventional red or blue light-activated treatment and is equally effective, consultant dermatologist Sally Ibbotson (Ninewells Hospital, Dundee) told
a satellite meeting. PDT is based on the activation of light-sensitive agents (usually 5-aminolevulinic acid or methyl aminolevulinate) in diseased tissue to produce reactive oxygen species and consequent cell death. Actinic keratoses are common, pre-invasive cancerous lesions in sun-exposed skin.
A proportion of AKs progress to squamous cell carcinomas. Daylight PDT has now been in use in Scotland for a couple of years. A specialist nurse applies the photosensitiser solution to the area of skin to be treated €“ typically on the head and neck €“ and the patient is exposed to sunlight for two hours. The entire area under treatment is also covered with a high-factor sunscreen to prevent burning by UV light.
This has to be a non-reflecting sunscreen that does not contain zinc oxide or titanium dioxide as these will reduce the amount of visible light reaching the skin.
Dr Ibbotson acknowledged that dPDT can only be delivered in Scotland between April and October. Even then, one patient had needed two hot water bottles to keep warm while undergoing treatment in the garden, she said.
Another study, presented by Dr Susan O'Gorman (St Vincent's University Hospital, Dublin) showed that a white light-emitting diode was equally effective and could provide a year-round treatment option.
Meeting patients' psychological needs
It is important to recognise that the psychological and social impact of skin conditions extends above and beyond the outward signs and symptoms. Psoriasis, for example, exerts a negative burden on health-related quality of life, which is equivalent to chronic, severe conditions such as ischaemic heart disease, diabetes, depression and even cancer.6 Chronic skin conditions, such as psoriasis and eczema, often engender embarrassment among sufferers and there may be strong feelings of stigmatisation due to the outward visibility of the skin lesions.
There is also a large, time-consuming treatment burden, with topical treatments typically requiring regular application, several times daily, every day, often for years.
Preparations for skin conditions may be messy, strong smelling, staining to the skin and clothes, and generally difficult to use. For most customers with a skin condition, the overriding issue will be the unsightly appearance of their skin complaint, the negative attention it attracts from others and the effect this has on their quality of life.4
Experts at the British Association of Dermatologists (BAD) suggest that sufferers take proactive steps to educate and inform those around them about their skin condition, pointing out that €a simple explanation will often turn their misconceptions into support€. Pharmacists can offer reassurance to patients by explaining the cause and prognosis of their condition, stressing the non-infectious nature of most chronic skin complaints, and highlighting the positive improvement in symptoms that can be achieved with treatment. Pharmacy staff also have an important part to play in directing customers to key external sources of support, such as charities and patient groups.
According to the King's Fund report: €Pharmacies could play an increasing role in signposting patients to information, treatment and to further healthcare advice if needed. This is particularly important as many patients with chronic skin conditions (like psoriasis) 'drop out' of primary care and specialist care services and seek treatment themselves.€
In terms of making everyday life easier for customers with skin conditions, the pharmacy can help by providing advice on the optimal application of topical products and encouraging treatment compliance. Sticking to a prescribed regimen, or creating a bespoke daily routine for the application of topical treatments that is as unobtrusive as possible, may help patients cope with the monotony of ongoing treatment.
The chronic nature of many skin conditions also emphasises the need for medicines management support to improve overall outcomes for those with dermatological disorders.3 At a practical level pharmacists can help patients with skin conditions get maximum benefit from their prescribed medications and any regularly used OTC self-care products by carrying out a MUR.
Detecting skin cancer
 Although mortality from skin conditions as a whole remains relatively low, skin cancer rates in the UK are rising and half of all specialist dermatology activity is now taken up with the diagnosis and management of skin lesions.2
Although mortality from skin conditions as a whole remains relatively low, skin cancer rates in the UK are rising and half of all specialist dermatology activity is now taken up with the diagnosis and management of skin lesions.2
Basic warning signs of potential malignancy to look out for on the skin include a skin growth (of any colour) that increases in size; a mole that appears different to other moles; and a mole, birthmark, beauty mark or any brown spot that varies in colour, increases in size or thickness, changes in texture, is irregular in outline, is larger than the size of a pencil eraser, or appears after the age of 21 years. Customers should also be aware of any new red or darker colour flaky, raised patches of skin, a new fleshcoloured firm lump, an open sore that fails to heal and/or a spot or sore that is persistently itchy or painful, crusts over or bleeds.
It is also important to encourage people to check their moles regularly using the ABCDE mnemonic:
- Asymmetry: differing shape to the two halves of a mole
- Border: irregular, blurred or notched edges of a mole
- Colour: uneven colour with different shades of black, brown and pink visible
- Diameter: most melanomas are at least 6mm in diameter
- Expert: if in any doubt, the person should see their GP for further investigation.
The skin cancer charity Skcin provides a downloadable body map which patients can use to record their findings.
References
- The British Skin Foundation
- The King's Fund. How can dermatology services meet current and future patient needs while ensuring that quality of care is not compromised and that access is equitable across the UK? Report published 7th March 2014. Available at: bad.org.uk/shared/get-file.ashx?id=2347& itemtype=document
- Tucker R & Duffy J. The role of community pharmacists in the management of skin problems. J Pharma Care Health Sys 2014; 1:105
- British Association of Dermatologists
- British National Formulary
- Lee & Thomson. Adverse Drug Reaction 2nd Edition. Chapter 5, p125-156: Drug-induced skin reactions. Pharmaceutical Press 2006

