What's new in COPD & asthma care (part 1)
In Learning
Follow this topic
Bookmark
Record learning outcomes
There could be up to 2 million people living with COPD that is undiagnosed, so what symptoms should pharmacists look for and when should suspected cases be referred to a GP? In the first of two articles, we look at how COPD is diagnosed.
Key facts
- COPD accounts for about one in 20 deaths, according to the British Lung Foundation
- Around 1.2 million people have been diagnosed with COPD, but the true number of sufferers could be over 3 million
- Acute COPD exacerbations are the second commonest reason for emergency hospital admissions

Suffering from chronic obstructive pulmonary disease (COPD) can have a dramatic impact on someone's quality of life.
€Around July 2012, I noticed that I would get incredibly breathless doing everyday tasks €“ walking around the house, getting out of bed, getting dressed, even talking on the phone €“ but I brushed it off,€ says Simon Pearce, a 41-year-old Londoner. €Then in November 2013, after a visit to the GP, I was diagnosed with COPD. It is hard as COPD is an invisible illness that is not immediately obvious. The reality is that simple things like walking up the stairs can leave you feeling like you have run a marathon.€
Over recent years, several new COPD treatments have reached the market €“ helping to drive awareness and offering new management options €“ although a cure remains as elusive as ever. Eventually, breathlessness can emerge at rest and, tragically, COPD often proves fatal. Indeed, COPD accounts for about one in 20 deaths (5.3 per cent), according to a British Lung Foundation (BLF) estimate.
€We recognise the central role of pharmacists in tackling COPD and asthma,€ says Ashley Green, BLF head of service development. €Pharmacists are in a unique position to support the diagnosis of COPD, raise awareness and optimise treatment.€
Common condition
According to the BLF, some 1.2 million people in the UK have diagnosed COPD. Yet most cases don't come to a healthcare professional's attention until the patient is admitted to hospital.
€There is a huge mismatch between the number of people who have been diagnosed and those living with COPD in the community,€ says Green. €The true number of people with COPD in the UK could be 3 million or even higher. Pharmacists have an important role in raising awareness of COPD symptoms among patients and referring suspected cases to GPs. It is essential that we diagnose more people when they still have early COPD. All too often, COPD is first diagnosed when a person is admitted to hospital with a severe exacerbation.€
Certain people do seem to be especially likely to develop COPD. A study from Imperial College, for example, mapped patterns of asthma and COPD across England. People in the North €“ including Liverpool, Manchester, Leeds, Sheffield, Newcastle and Durham €“ were most likely to experience chronic respiratory diseases.
Several factors may contribute to the variations across the UK, including deprivation, air pollution, smoking1, and genetic and cultural differences.2 For example, a study of 358,614 patients from 47 general practices in London reported a COPD prevalence of 1.55 per cent in white people, 0.78 per cent in Asians and 0.58 per cent in black people. After adjusting for smoking, Asian and Black people were 18 and 56 per cent less likely to develop COPD than white people.2
Diagnosing COPD
COPD encompasses three elements:
€¢ Emphysema
€¢ Bronchiolitis
€¢ Bronchitis.
Emphysema follows the progressive destruction of the alveoli, which limits oxygen uptake and carbon dioxide release.
The elastin fibres that keep the small airways open are destroyed, so these collapse, trapping air in the lungs leading to over-inflation, especially during exercise.3 In bronchiolitis, smaller airways become inflamed and scarred (fibrotic). Indeed, 'pruning' of small airways can occur before lung function changes. COPD patients often show bronchitis, the excessive production of mucus, which may be purulent, especially during exacerbations.3
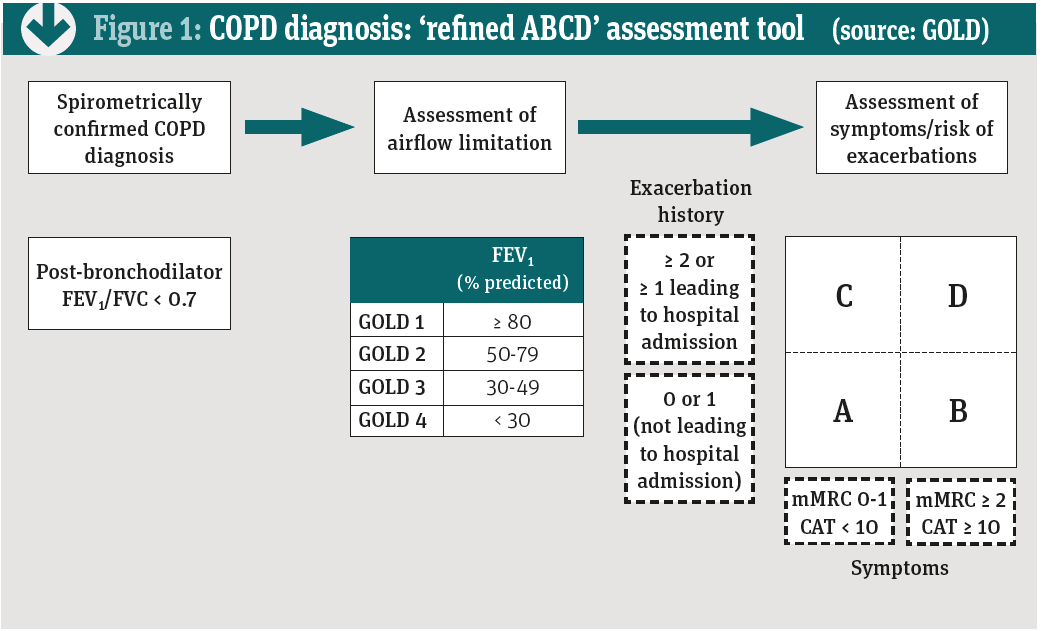
To improve COPD care, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) has published guidelines covering diagnosis, management and prevention since 2001. The latest version was released in March. These new guidelines suggest considering COPD in patients who present with dyspnoea, chronic cough or sputum production, and/or a history of exposure to risk factors. A formal diagnosis depends on spirometry €“ specifically a ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) of less than 0.7 (see table below).
Cough, GOLD notes, is often the first COPD symptom. Eventually, up to 30 per cent of COPD patients develop cough with sputum. €Pharmacists should refer anyone with a history of chronic cough, repeated chest infections and breathlessness to their GP,€ Ashley Green says. €However, COPD often goes undiagnosed, partly because patients and GPs might blame the symptoms on age or smoking and partly because many practices don't have a spirometer or a nurse trained in its use.€
The BLF supports several initiatives that include pharmacists, including working with CCGs to run screening events to detect COPD.
€Many people with COPD do not raise the symptoms with their GP,€ Green says. €They think that the symptoms are just part of getting older or because they smoke. Pharmacists can help raise awareness about COPD symptoms and, when appropriate, refer to GPs. Pharmacists can also watch for clues, such as a large number of prescriptions for short-acting bronchodilators or antibiotics, or repeatedly buying cough mixture.€
The economic burden of COPD
The BLF estimates that COPD costs the UK economy £49bn a year. Direct costs account for £1.8bn, indirect costs (e.g. lost productivity) for £61m and intangible costs (e.g. pain, suffering and excess mortality) for £46.6bn. The total cost associated with COPD is more than double that arising from asthma (£21.6bn), largely reflecting COPD's larger intangible costs (£18.5bn for asthma). COPD also exceeds the direct costs (£163m) and total costs (£45.9bn) imposed by cancers of the trachea, bronchus and lungs.
Diverse disease
COPD is a diverse disease, so GOLD now also divides people with a FEV1:FVC ratio of <0.7 based on the percentage FEV1 of predicted (see Figure 1, previous page):
€¢ GOLD 1: ‰¥80
€¢ GOLD 2: 50-79
€¢ GOLD 3: 30-49
€¢ GOLD 4: <30
The assessment further stratifies patients based on exacerbation history:
€¢ No exacerbation or one exacerbation in the last year that did not lead to an admission
€¢ ‰¥2 exacerbations in the last year or ‰¥1 exacerbation leading to hospital admission.
Finally, the assessment splits people based on symptoms and exacerbation risk:
€¢ A score on the modified Medical Research Council dyspnoea scale (mMRC) of 0-1 and a COPD assessment test (CAT) score of <10. CAT assesses the impact on health status
€¢ A mMRC score ‰¥2 and CAT score of ‰¥10.
Take two patients €“ Dave and Alex. Both have FEV1 <30 per cent of predicted and CAT scores of 18. Dave did not experience any exacerbations in the past year but Alex experienced three. In the previous version of the guidelines, Dave and Alex would both be GOLD D. Now Alex would be GOLD grade 4, group D and Dave GOLD grade 4, group B.
COPD causes more than just dyspnoea (difficult or laboured breathing). Patients often endure repeated chest infections and serious co-morbidities such as cardiovascular disease (CVD) and conditions affecting the kidneys, metabolism and the central nervous and musculoskeletal systems. About half of COPD patients die from CVD including right heart failure, pulmonary hypertension, stroke, myocardial infarction and DVT.3
Exacerbations drive much of the morbidity and mortality associated with COPD €“ about 8 per cent of people admitted with acute COPD exacerbations die in hospital, for example, while 23 per cent die within one year. Acute COPD exacerbations are the second commonest reason for emergency hospital admissions
in the UK.4
New research presented at the recent American Thoracic Society conference suggests that people with a history of, or at risk of, CVD seem more likely to suffer a MI or stroke after an acute COPD exacerbation.
Researchers analysed 16,485 current and former smokers with COPD between 40 and 80 years of age who had CVD or multiple risk factors for CVD. The risk of MI or stroke was nearly four-fold higher (hazard ratio [HR] 3.8) during the 30 days after an acute exacerbation and was almost double (HR 1.8) between 31 days and a year after the exacerbation. After this, the risk was not significantly different.
€Previous studies have shown that lower lung function, such as occurs with COPD, is a risk factor for CVD,€ says Ken Kunisaki, associate professor of medicine at the University of Minnesota. €One theory for why this happens is that COPD triggers inflammation and that, in turn, leads to CVD. Because COPD exacerbations lead to particularly high levels of inflammation, we wondered if these exacerbations would be linked to higher rates of CVD events.€
The findings might change treatment. €One approach might be to study currently used cardiac medications, such as antiplatelet agents, statins and/or beta-blockers immediately following COPD exacerbations,€ says Dr Kunisaki. €Another approach might be to use experimental drugs that specifically reduce inflammation.€ Until studies identify effective interventions, patients who recently experienced a COPD exacerbation €should pay attention to and seek immediate care€ for symptoms of heart attack or stroke.
The GOLD guidelines also advise healthcare professionals to actively seek and treat chronic co-morbidities. The guidelines note, for example, that fatigue, weight loss and anorexia are common in severe and very severe COPD and can influence prognosis. These symptoms may also arise from other conditions, including tuberculosis and lung cancer €“ so pharmacists should refer people with fatigue, weight loss or anorexia for further investigation.
Exacerbations drive much of the morbidity and mortality associated with COPD
Pharmacists and asthma

According to Asthma UK, 5.4 million people receive treatment for the disease in the UK, 80 per cent of whom are adults. Yet, four in five people feel that their asthma is poorly controlled and three people die each day from asthma. Two of these deaths could have been prevented.
Against this background, increasing evidence suggests that pharmacists can improve outcomes. One study enrolled 248 people with asthma from 30 community pharmacies in Australia. Patients with poor asthma control were almost 2.58 times more likely to have had a 'life-threatening asthma attack' in the previous five years than those with good asthma control and 2.74 times more likely to make an 'emergency medical presentation'. Yet 70.8 per cent of the patients felt that their asthma was well or completely controlled.5
Similar results emerged in the Annual Asthma Survey 2016: 82 per cent of people felt their asthma was poorly controlled but just 15 per cent felt their asthma care was poor. Inaccurate perceptions of asthma control might mean that patients are unlikely to proactively seek help. Community pharmacists are well placed to address these issues by directly speaking to patients.5
NMS reviews can help address poor adherence. A study performed at 46 community pharmacies in England assessed the effect of the NMS on adherence in 504 people with asthma, COPD, hypertension, type 2 diabetes or taking an anticoagulant or antiplatelet. After adjusting for confounders, the NMS increased the likelihood of adherence by 67 per cent.6
Asthma self-management €“ which includes several elements pharmacists can facilitate such as patient education, developing an action plan and regular review €“ seems to improve outcomes, according to 27 previous systematic reviews encompassing 257 RCTs. The proportion of patients hospitalised declined from 7.2-25.9 per cent (depending on the study) to 4.6-14.0 per cent.
The proportion attending A&E declined from 19.4-30.7 per cent to 13.1-22.4 per cent. The proportion of patients making unscheduled consultations declined from 36.6 to 24.9 per cent in one meta-analysis and from 22.0 to 14.3 per cent in the other.7
Self-management also seems to improve asthma control and quality of life. For example, six out of 10 reviews reported that self-management reduced symptoms. The other four reviews examining symptom control reported inconsistent results or no benefit.7 Asthma may be common, but there is still clearly considerable unmet need that pharmacists can help address.
Next month: therapeutic management of COPD.
References
1. Boulieri A, Hansell A, and Blangiardo M. Investigating trends in asthma and COPD through multiple data sources: A small area study. Spatial and Spatio-temporal Epidemiology 2016; 19:28-36
2. Gilkes A, Ashworth M, Schofield P et al. Does COPD risk vary by ethnicity? A retrospective cross-sectional study. Int J Chron Obstruct Pulmon Dis 2016; 11:739-46
3. Anderson G. Advances in understanding COPD F1000Research Published: 27 Sep 2016 doi: 10.12688/f1000research.7018.1
4. Rothnie KJ, Mullerova H, Thomas SL et al. Recording of hospitalizations for acute exacerbations of COPD in UK electronic health care records. Clin Epidemiol 2016; 8:771-782
5. Watkins K, Bourdin A, Trevenen M et al. Opportunities to develop the professional role of community pharmacists in the care of patients with asthma: a cross-sectional study. Npj Primary Care Respiratory Medicine 2016; 26:16082
6. Elliott RA, Boyd MJ, Salema N-E et al. Supporting adherence for people starting a new medication for a long-term condition through community pharmacies: a pragmatic randomised controlled trial of the New Medicine Service. BMJ Quality & Safety 2016; 25:747-758
7. Pinnock H, Parke HL, Panagioti M et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Medicine 2017; 15:64
Further resources
€¢ British Lung Foundation: psnc.org.uk/our-news/new-resources-from-blf
€¢ Global Initiative for Chronic Obstructive Lung Disease: goldcopd.org
