Is hub and spoke really the answer for pharmacy?
In Analysis
Follow this topic
Bookmark
Record learning outcomes
The Government wants community pharmacies in England to adopt hub and spoke dispensing models €“ but is this feasible across the network on a large scale?
The letter issued jointly by the Department of Health and NHS England before Christmas on December 17 said that the Department would consult on changing the Human Medicines Regulations (2012) €to allow all pharmacies to access the efficiency created by 'hub and spoke' dispensing€.
But can anyone actually tell us what is meant by 'hub and spoke'? At the moment, it is a phrase that people with different perspectives and agendas are using €“ with some using it to refer to dispensing hubs and others to centralised dispensing.
The Oxford Dictionary's definition of dispensing in relation to medicines is: €To make up and give out medicine according to a doctor's prescription.€ So what we are really referring to in a hub is centralised or remote assembly, not dispensing, which includes supply to a patient, whether that is face-to-face in a pharmacy or to their home (i.e. the 'spoke' element). It is that patient interaction that creates the opportunity for an intervention, whether to support the safe and appropriate use of medicines or provide advice and support on healthy lifestyles.
Recap: how it all started...
In 2013, NHS England's Call to Action consultation1 suggested greater use of technology and automation to improve efficiencies and reduce errors. In its response, Pharmacy Voice called for the relaxation of the regulations to create a level playing field for independents so that they too could embrace technological advances.2
NHS England's Five Year Forward View3 (5YFV) is Simon Steven's plan to save the NHS, which aims to move more care into the community through integration; support innovation and technology; enhance quality; and improve efficiencies and utilise the skills and accessibility of pharmacy to a greater extent.
Everything went quiet for a while until the chief pharmaceutical officer for England, Dr Keith Ridge, told the Royal Pharmaceutical Society's conference in September 2015 that he wanted all community pharmacies to be legally allowed to operate a hub and spoke model €as soon as possible€. Such facilities could be capable of dealing with two-thirds of the dispensing volume in England, he said, in addition to making dispensing €more efficient and safer€ and €freeing up highly trained staff to work with patients€. The future €is clinical€, he said, €and underpinned by efficient and effective use of technology€.
These views have now started to move closer to reality. In the letter4 issued jointly by the Department of Health and NHS England in December, plans were outlined to consult on changes to the HMR 2012 legislation to enable hub and spoke dispensing in 2016 plus some controversial reforms to funding and a review of access and integration for community pharmacy.
Context
Some of the larger multiple groups have been operating hub and spoke systems for many years to release capacity in some of their pharmacies, particularly for care home supplies and domiciliary monitored dosage systems. However, this has only just started to scale up for repeat medication, with LloydsPharmacy, Boots and, more recently, Day Lewis announcing further intentions (see below).
The current legislation in the Human Medicines Regulations (2012) prevents a hub and spoke approach taking place between different business entities, thus limiting the potential opportunities for independents to consider using the option.
The proposals raise many questions, such as:
- Where is the evidence that hub and spoke dispensing improves cost-effectiveness?
- Who does what and how in a non-integrated model and how will the finances work?
- Who owns the stock?
- Who gains any retained margins on the stock?
- How will the technology and communication work and information governance be assured?
- Who owns the patient EPS nomination and PMR data?
- How is the funding remodelled to incentivise and appropriately reward services rather than supply management?
- What does success look like and what are the measures?
GPhC view
The General Pharmaceutical Council's view is that this is an area for legitimate debate, but any change to HMR 2012 is a public policy decision. It is a business decision how pharmacies organise themselves within the legal framework and professional standards, says Duncan Rudkin, chief executive and registrar. However, a hub and spoke operation would require a complex set of standard operating procedures to be put in place first.
The GPhC issued guidance for pharmacies providing services at a distance in April 20155, which has some implications for remote assembly. However, Duncan Rudkin says there are still many questions that need answering, including:
- What are the risks and opportunities for the public in doing this and can they be managed to ensure safety for patients?
- Who is accountable and responsible for each element? (This is no different for single or multiple business entities)
- In relation to the current Standards for Registered Pharmacies, who does what, where do they do it and where does the buck stop?
While everyone agrees that things have to change, there seems to be no consensus among the various parties on what that change should entail.
Detrimental
Sue Sharpe, PSNC chief executive, believes that regulations to permit remote assembly of medicines could have a benefit for pharmacies as a means of outsourcing some of the workload of dispensing and stock management.
€There may be some scope for the [regulations] to free up time within the pharmacy team to provide support to patients,€ she says, €but it is important that all sectors of pharmacy are able to explore the option.€
The fear, she points out, is that there are those who see this as an opportunity to replace the community pharmacy service with a remote supply operation. This would be extremely detrimental. Most people on regular medication value the accessibility and support they can get from their local pharmacy.
This could also send the development of community pharmacy services into reverse and lead to unknown levels of increased demand on more expensive services in primary care €“ GP appointments and urgent care.
Rob Darracott, Pharmacy Voice chief executive, is clear that pharmacy and the NHS regards hub and spoke as remote assembly (hub) with the originator pharmacy being the spoke, and not home delivery (central dispensing). The spoke is where the clinical care is provided and is the final step in the supply chain of dispensing, he says.
€Utilising technology and lean practice to enable hub assembly would release capacity in the 'spoke' pharmacy for more clinical services and improved safety and adherence, as well as patient experience and outcomes.€
Lean thinking at Mayberry Pharmacy
Paul Mayberry is managing director of the Mayberry Pharmacy group of seven pharmacies in South Wales. Paul began several years ago to explore lean principles in order to work smarter and reduce waste within his group.
Realising that the most expensive, but important, assets were his employees, particularly his pharmacists, Paul developed his skill mix with ACTs and added a robot at one of his branches €“ the hub. €It required a big shift in mindset to overcome resistance to change and new ways of working,€ says Paul. €The robot and the hub constantly got the blame whatever went wrong.€
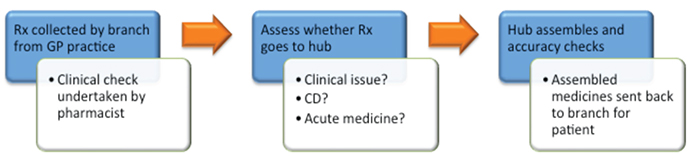
Initially, there were major IT challenges with difficulties accessing patient records but their PMR provider resolved these with central access. The diagram illustrates the flow at Mayberry Pharmacy, with up to 60 per cent of prescriptions going to the hub.
Over time, the teams understood the benefits of releasing time to deal with more complex queries, improve the patient experience through better pharmaceutical care and new services such as their blood pressure initiative. This all led to better job satisfaction, with different personnel more suiting the hub roles and others the patient-facing ones.
Paul says he would do it all again. €We learnt a lot on the way and we now have a culture of lean thinking embedded in the organisation.€ He was able to reduce his stockholding by 35 per cent but did not reduce his employee numbers, using the released time to grow his business.
Central dispensing at Day Lewis
The Day Lewis Pharmacy group recently announced that it was to expand the use of its central dispensing unit (CDU) to the whole group as part of its overall Healthy Living Pharmacy strategy. The aim is to:
- Release time and capacity for better patient care
- Deliver more services
- Improve safety yet further
- Motivate its pharmacy teams
- Grow the business without expensive refits, relocations or increasing staffing levels.
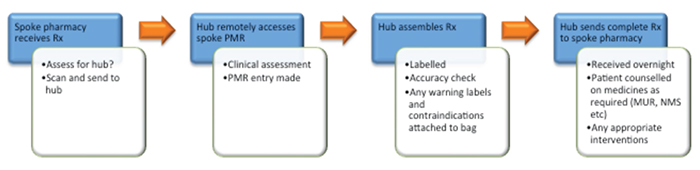
The process for Day Lewis is currently as follows:
Tipping point
British Association of Pharmaceutical Wholesalers executive director Martin Sawer wonders if NHS England is seeing hub and spoke as a panacea to contribute to the filling of its £22bn funding black hole or truly an opportunity to improve patient care by releasing time at the coalface.
Technology is reaching a tipping point and will need to be embraced by all, he says, €but it has to be a commercial decision, which will be different for vertically integrated organisations and the independent sector, should regulations change. The transformation certainly cannot happen overnight.€ He also points out that hub and spoke cannot be used for controlled drugs, cold-chain products and acute prescriptions, and may only work in urban, not rural, areas due to the costs of the logistics.
Howard Duff, RPS director for England, confirmed that the RPS has yet to agree a policy on hub and spoke but is €currently considering all aspects of remote assembly and dispensing with a policy position and professional standards available in early 2016€.
Automation and technology is here and has to be embraced, he says, with pharmacy challenged with capacity issues, reduced funding and increasing costs. However, he cautions that there is a risk of direct supply to patients bypassing the community sector and losing the important patientpharmacist interaction.
€We cannot keep doing what we have always done €“ dispensing large volumes of prescriptions at low margins,€ says Cormac Tobin, managing director of Celesio UK. He prefers the term 'centralised dispensing' to hub and spoke. Celesio uses a Prescription Assembly Solutions (PAS) unit in its Warrington warehouse. While results are still being evaluated, early indications are that error rates are down (every activity in the process is tracked and checked using technology).
However, while it does free up time (approximately 30-50 per cent of volume being moved to the hub) and reduce stock holding, there is no evidence yet of actual cost savings. The complex scenario facing pharmacy is best illustrated by a force field analysis (see Figure 1). The green arrows indicate the benefits and the red arrows the risks, with the size of the arrow depicting the scale.
While it is not science-based, such an analysis reflects the various perspective and insights. One thing is for certain. Given everything else that is going on, doing nothing is not an option.
Mike Holden is principal associate at Pharmacy Complete
