Improving treatment of constipation
In Clinical
Follow this topic
Bookmark
Record learning outcomes
There is an urgent need to improve bowel care and the management of constipation, not only to relieve patient distress, but also to reduce NHS treatment costs and expensive, non-elective admissions

Key facts
• It is estimated that around one in seven adults, and up to one in every three children in the UK, has constipation at any one time
• In 2018-19, 76,929 people in England were admitted to hospital with constipation, equivalent to 211 people a day. Of those, around three-quarters were unplanned emergency admissions
• NHS England spent £168m treating constipation in 2018/19. This includes avoidable admissions to A&E for constipation (£81m) and prescription laxative costs (£87m)
• The total cost is much higher when GP visits, home visits and OTC laxatives are taken into account
Inadequate management of constipation has a significant impact on the over-burdened National Health Service. In 2018-19, £168m was spent by NHS England on treating constipation. To put this figure into perspective, this is equivalent to the cost of funding 7,304 newly qualified nurses for a year. In reality, the total cost is likely to be much higher if GP visits, home visits and OTC laxatives are factored in.
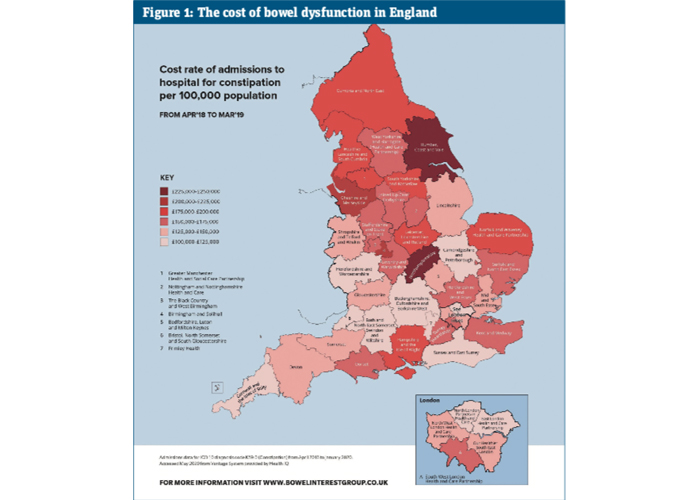
Further analysis of the scale of the problem across England reveals variation in the cost of admissions per region (see Figure 1). Humber, Coast and Vale, Cheshire and Merseyside, and Birmingham and Solihull have the highest rate of admissions in the country, with the highest rate reaching 209.6 per 100,000 population. At the lower end of the scale, we find North London Partners in Health and Care, East London Health and Care Partnership, and Bristol, North Somerset and South Gloucestershire. The latter region records the lowest rate at 82.8 per 100,000 population.
Looking at trends from 2016/17 to 2018/19, not one region has seen a year-on-year reduction in the spend on laxatives or admissions for constipation. To begin addressing this issue, there must be a national change in the diagnosis and management of constipation throughout the NHS.
As might be expected, areas with a higher spend on laxatives tend to see higher rates of admission – so improving bowel health could potentially produce a double benefit in reducing both admissions and treatment costs.
Not one region has seen a year-on-year reduction in spend on laxatives or admissions for constipation
Causes of constipation
Addressing the causes of constipation and underlying conditions that aggravate symptoms is essential to improve patient comfort regardless of whether treatment is recommended. The first step is to assess aspects of modern daily living that can contribute to constipation.
Constipation is associated with environmental stressors, which are increasingly experienced by the population. Insufficient exercise and fibre-poor processed food are two common lifestyle factors that may be behind the symptoms, while overfilled schedules can hinder a regular, unhurried toilet routine, which is essential for good bowel health.
Constipation may also be caused by certain drugs, such as opiates, antihistamines and antidepressants. In these instances, healthcare professionals are advised to take a preventative approach where possible, for instance, by co-prescribing a laxative when starting a patient on a medication that is known to cause constipation.
Co-existing medical conditions, such as neurological disorders or diabetes, further increase the likelihood of developing symptoms.
While most patients have ‘functional’ constipation, where they experience symptoms without any underlying non-bowel problems, patients with conditions including spina bifida, multiple sclerosis or Parkinson’s disease often develop neurogenic constipation. Many patients with neurogenic bowel dysfunction spend a significant part of their day on bowel management, with up to 63 per cent spending more than one hour on each episode.
Women are twice as likely to have constipation, for a number of reasons, including pregnancy and pelvic floor disorders. Sixty per cent of constipation-related hospital admissions are female, although it is likely that this also reflects the willingness of women to seek healthcare. Elderly patients are disproportionately affected by constipation as they are more likely to have reduced mobility, suffer from medical co-morbidities or be taking medications. However, it is incorrectly assumed that constipation is inevitable in old age, and its prevalence in this population group may be reduced with improved management.
While older patients may be particularly reluctant to discuss bowel health, embarrassment about constipation is a wider issue. A YouGov survey of over 2,000 people found that nearly a fifth said they would feel embarrassed talking to their GP about constipation and would try and solve it themselves, without speaking to anyone about it. Over time symptoms can impact quality of life and lead to anxiety or even depression, in addition to physical discomfort.
Resources for treating constipation
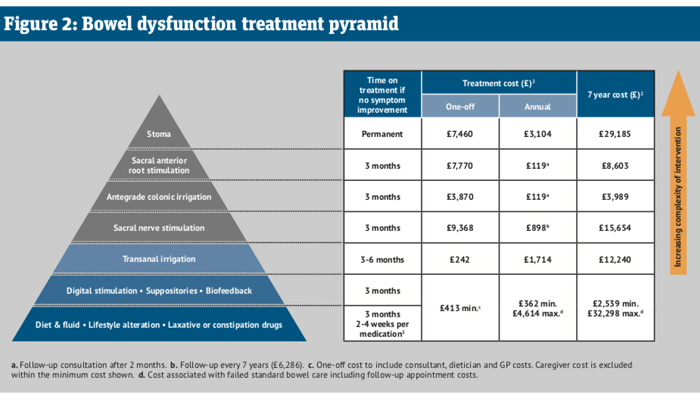
Patients are often treated empirically with laxatives, and there is a lack of guidance on how, when, or with which therapeutic alternative to progress treatment. As part of its work raising awareness about constipation treatment, the Bowel Interest Group has produced a simple diagram of treatments that can be prescribed once adjusting diet, fluid intake and lifestyle, and taking laxatives or other constipation drugs, is no longer effective.
Based on the NICE Clinical Knowledge Summary, the bowel dysfunction treatment pyramid shown in Figure 2 indicates the recommended length of time that each therapy should be tested before moving to the next treatment option. It also indicates the one-off and longer-term costs of each option, calculating that standard starting treatment can cost up to £32,298 over seven years if practitioners do not prescribe more effective treatment.
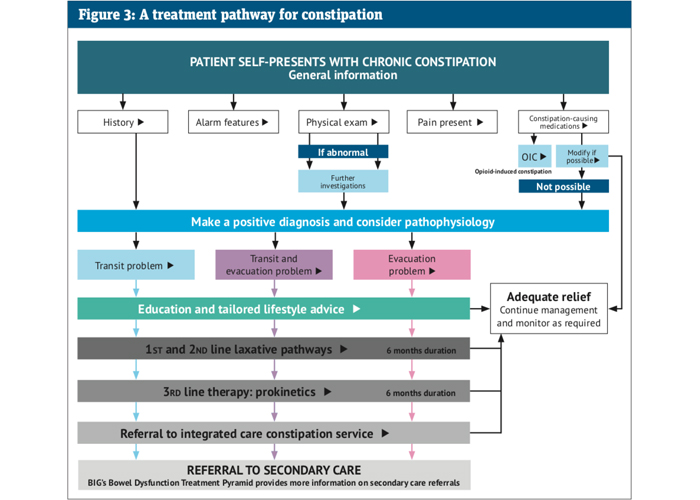
To guide the prescribing process, the Bowel Interest Group has also produced an interactive treatment pathway, which starts at the initial consultation through to third-line therapies and when to refer to secondary care (see Figure 3). As the lack of supporting information is a particular concern at a primary care level, this resource is structured to enable quick and safe decision-making. Practitioners can click through the pathway to the relevant section during a patient consultation.
Outside the GP surgery, the availability of OTC laxatives can lead to overuse and misuse by patients. Last year, a review of non-prescription stimulant laxatives led to new measures from the MHRA, restricting pack sizes, revising recommended ages for use and introducing new safety warnings (see CPD module on p15 for more detail). Among the agency’s concerns were “evidence of misuse by people with eating disorders, and of long-term use by the elderly, as well as inappropriate use in children”.
This further highlights the need for greater awareness among the wider population about the use of laxatives, as well as constipation symptoms and their treatment.
Common and intrusive
Constipation is often perceived as a minor issue and yet it is a common and intrusive problem, with a substantial cost to the health service. Reducing the prevalence of chronic conditions is particularly important against the backdrop of the current pandemic. As the NHS is likely to make significant changes to service provision in the wake of Covid, this is an opportunity to both improve patient outcomes and make savings through early evidence-based treatments.
Local initiatives are already in place. Individual trusts have developed bowel management pathways allowing patients to be triaged from, for example, emergency departments directly to clinics that deal with constipation, and in turn this can lead to a reduction in admissions. Clinical commissioning groups in the North East, which are the highest prescribers of laxatives in England, are working with medicines optimisation teams to address this issue within the region. However, there must be a large-scale adoption of such measures and services for there to be a national change.
Reference
• Bowel Interest Group: Cost of Constipation Report 2020.