Cough, cold and the flu vaccine
In OTC Category Reviews
Follow this topic
Bookmark
Record learning outcomes
The Covid-19 vaccine is understandably being heralded as the next big breakthrough in healthcare, but it is important to not lose sight of another vaccine that prevents a huge amount of illness every year
The seasonal flu immunisation programme is always important, but never more so than now. Many of those who are at risk of the serious complications of flu are also regarded as vulnerable to the effects of Covid-19. With the latter still circulating, it is essential that as many people as possible are protected from the former by making sure flu vaccination rates hit record levels.

This year’s flu jab programme is one of the most complicated thus far. More groups than ever are eligible for an NHS vaccination, with household contacts of individuals on the NHS shielded patients list, Year 7 children, and health and social care workers looking after patients who are still living in their own homes (known as domiciliary care) being added to an already long list (see panel below). There is also an ambition to extend the programme from November onwards to include adults aged 50-64 years, though this is subject to having enough vaccines still available.
The overall aim of the programme is to vaccinate at least 75 per cent of individuals in the majority of eligible groups, and to offer immunisation to every single frontline health and social care worker.
Various vaccines
Another consideration is the number of different vaccines available, with the product administered dependent on the group to which the patient belongs:
- QIVc (quadrivalent influenza vaccine, cell-culture) is the first choice for eligible adults aged 18-64 years, including pregnant women. It is also an alternative for children aged nine years or older who cannot have the LAIV vaccine outlined below
- QIVe (quadrivalent influenza vaccine, egg-grown) is first choice for eligible children aged six months to less than two years and is an alternative to QIVc for adults aged 18-65 years and to LAIV for children under nine years, as well as older children being vaccinated in a school setting
- LAIV (live attenuated influenza vaccine, also quadrivalent) is considered the most appropriate option for children from two years upwards and has the benefit of being administered nasally rather than being injected. However, it contains porcine gelatine so may be unacceptable to some families, in which case an alternative may be offered
- aTIV (adjuvanted trivalent influenza vaccine) is regarded as the most effective product for the over 65s, with QIVc suitable if it is not available.
All of these vaccines confer protection against two strains of influenza A and two strains of influenza B, with the exception of trivalent vaccines, which protect against two strains of influenza A a single influenza B strain.
The final complexity surrounding this year’s flu vaccination programme is that 2020 watchword: coronavirus. Guidance on social distancing, hand hygiene and use of personal protective equipment (PPE) should be adhered to, though it is worth noting that these documents state there is no need for items such as gloves and aprons to be used for clinical settings like vaccination clinics because the amount of contact with individuals is regarded as minimal. Patients are likely to need reassurance when they see the set up for immunisation clinics, particularly those who were advised to shield.
Over 1.7 million flu vaccinations were provided by community pharmacies in 2019/20
Perfect fit?
According to figures published by the NHS Business Services Authority, over 1.7 million flu vaccinations were provided by community pharmacies in 2019/20 – a near 20 per cent rise on the previous year. But with more than 30 million people included in the eligibility criteria for this year’s programme, the sector needs to make another huge leap forward in the interests of trying to reduce pressure on the health and social care system at a time when it is still healing from the impact of the Covid-19 pandemic, while, of course, protecting the most vulnerable.
Ade Williams, superintendent pharmacist at M J Williams Pharmacy in Bristol, says that all flu vaccination providers need to pull together to reach the Government’s ambitious target. “There is awareness from all involved that nobody can deal with the volume of flu vaccinations that need to be given on their own, let alone in a Covid-secure manner. Logistically, it is impossible,” says Ade. “We need to put to one side the entrenched views on how different providers such as GPs and pharmacies are in competition with each other and instead have sensible conversations about working together to vaccinate as many people as possible in the eligible categories.”
Eligible groups
The people eligible for an NHS flu vaccination for the 2020/21 season are:
• All frontline health and social care workers
• All children aged two to 11 years as of 31 August 2020
• All adults aged 65 years or over as of 31 March 2021
• Anyone aged six months to less than 65 years in a clinical risk group, such as those with:
o Chronic respiratory, heart, kidney, liver or neurological disease
o Learning disability
o Diabetes
o A weakened immune system due to disease such as HIV or treatments such as chemotherapy
o A body mass excess of 40 or higher.
• All pregnant women
• Household contacts of those on the NHS shielded patient list or who are immunocompromised
• Residents of long-stay care homes or other facilities where rapid spread is likely and will cause high rates of illness and death
• Carers
• Staff working in care homes, hospices or delivering domiciliary care
• Anyone else deemed by a healthcare professional to be at risk of serious complications or exacerbation of underlying illness from flu.
Once this phase has been completed, and subject to sufficient stocks of vaccine being available, all adults aged 50-64 years will also be eligible.

Broadening access
There is a big push to increase uptake in certain groups, with the Department of Health and Social Care stating: “It is essential to increase flu vaccination levels for those who are living in the most deprived areas and from BAME communities. We need to ensure equitable uptake compared to the population as a whole and help protect those who are more at risk if they are to get Covid-19 and flu. It will therefore require high quality, dedicated and culturally competent engagement with local communities, employers and faith groups.”
Those from black, Asian, minority and ethnic (BAME) groups are reportedly at a higher risk of Covid-19. Black males are thought to be 4.2 times more likely to die from Covid-19 and black females 4.3 times more likely when compared to white males and females, according to a report published in May 2020 by the Office for National Statistics.
Pharmacies, located in the very heart of the communities they serve, are well placed to lead on this, but Ade warns that it isn’t a given. “The only way to tackle it is to take responsibility for it. Find out your local story – which groups aren’t getting their flu jabs and why? Where are they and how can we as a team tackle it?” he says. “All staff need to be talking to everyone who comes in. Simply asking ‘are you having your flu jab?’ opens up conversations in which people will say what is stopping them, which could range from cultural aversions around injections to having read on social media that the jab causes flu or doesn’t work. Then use your leverage as trusted healthcare professionals to address these misconceptions in a friendly and relatable manner to help them change their mindset.”
Ade highlights the ability to go off-site as another way of broadening access. “Not everyone is going to want to come to the pharmacy, so we need to think about going into community centres, churches, mosques,” he explains. “Wherever we need to go to get it to the populations that need it.” But he adds that care is needed around the messaging. “Remember to try and tell people to get vaccinated, not to have ‘our vaccination’. That way they will view it as an essential health intervention rather than a service that the pharmacy is trying to promote.”
Demand versus supply
An important consideration is where individuals fit in who aren’t eligible for a free NHS flu jab. There are several factors that could present stumbling blocks: expansion of the eligibility criteria as already described; a proposed second phase that will see those aged 50-64 years able to access free NHS vaccinations, albeit at a later date; and, of course, increased demand, which in many cases will be fuelled by anxiety resulting from the Covid-19 pandemic.
Communication is key, and Ade says that the UK health departments need to step up quickly in this regard. “We know we have people wanting private flu jabs as we – and many other pharmacies – have done them in previous years, and we have tried to find out if we can get stock of vaccines outside those which are ringfenced for the NHS scheme,” he explains. “But so far, the suppliers are telling us that everything they have is reserved for those patients. It would be helpful to know from when, or even if, there will be any spare capacity so we can plan for and explain to those other customers who are asking.”
Short supply in the short-term doesn’t necessarily mean that non-NHS flu jabs won’t be available in time, Ade stresses. “Every year there are always providers who don’t manage to use all their vaccines. Nobody wants redundant stock so in a couple of months we will have a clearer picture of where many have surplus and providers who still have demand may be able to obtain this stock in the interests of vaccinating more people rather than the vaccines going to waste,” he says. “The NHS quite rightly wants us to prioritise those who are vulnerable to the effects of flu, but that doesn’t mean it is the sole priority because population-wide health protection is important too.”
However, Ade cautions against pharmacies seeing this as a commercial opportunity. “We must remember that we are healthcare professionals, and people trust us to look after them. Rather than rushing in, explain to people why they need to wait – the shielding that many people had to do to protect themselves from coronavirus means there is not only much higher awareness of health vulnerabilities, but also recognition that these vulnerabilities are not always visible – and they will understand.”

Planting the seed
Mahendra Patel, Royal Pharmaceutical Society national board member, feels that the stage is set for this year’s flu vaccination campaign to be a big success, given the high public demand and the Government and providers sharing an ambition to get to as many people as possible. Furthermore, he highlights the potential for far-reaching positive consequences. “There is a real opportunity here to explore and address health inequalities through working across all communities,” he says. “By reaching out and building confidence and relationships – particularly among groups that have traditionally been slow to access healthcare services, including those, at times, who are high risk for a wide variety of reasons – we can start to have conversations about long-term conditions and mental health to help people manage them better.”
The opportunities to support people who don’t fall into an at-risk group are also wide reaching. “The same is true of those people who aren’t eligible for an NHS jab but come in for a private flu jab, perhaps because they are anxious for themselves, but also maybe because they are looking after and want to protect older generations of their family who are staying at home,” Mahendra continues. “Again, we should make more of the glaring and obvious opportunity that presents in terms of talking to them about other matters relating to health and wellbeing, as they may then spread those messages to their family, extended family members and friends. It’s about getting people vaccinated, of course, but also about planting the seeds for better health outcomes for everyone.”
Spot the difference
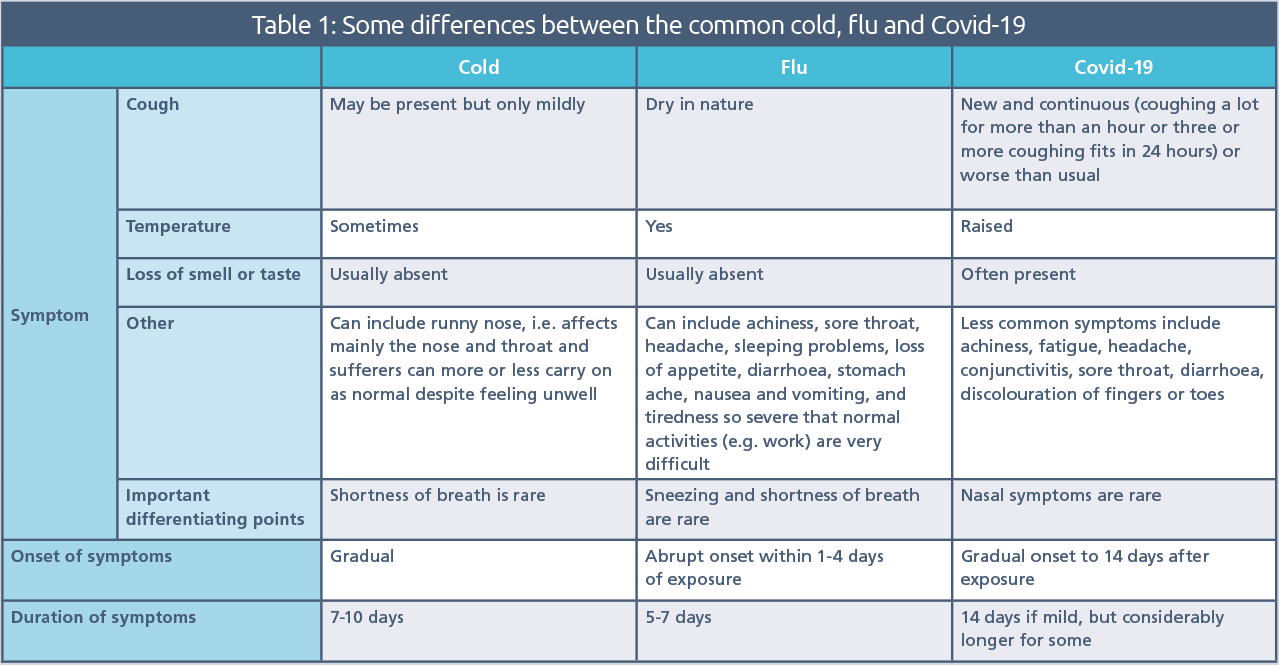
A cold, a bout of flu, an attack of Covid-19: all infections affecting the respiratory tract, but with subtle differences that pharmacy teams need to be aware of in order to provide the most appropriate advice.
Click on the table to see a larger version
IMPORTANT!
It’s vital to remember that these lists are not exhaustive and while these differences may be largely true on paper, respiratory illnesses will affect individuals in different ways. When it comes to Covid-19, the right and only approach is to refer anyone with the ‘red flag’ symptoms – a high temperature, a new and continuous cough, or a loss or change to the senses of taste and smell – for a test as a matter of urgency. They must isolate at home, other than to get a test, and not have visitors until a test result is received. Anyone they live with, and anyone in their support bubble, must also isolate until the test result is received. If this result is positive, they must self-isolate at home for at least 10 days after the onset of symptoms. For the latest advice, see NHS: coronavirus.