In Opinion
Follow this topic
Bookmark
Record learning outcomes
Community pharmacies are far more than dispensaries. They are the most accessible part of the NHS, handling millions of patient interactions every week, and pharmacists have become integral to modern primary care. No appointment, no waiting list, just expert clinical advice and the reassurance of human interaction.
Services such as Pharmacy First, contraception provision, hypertension detection and vaccination programmes are now a routine part of community pharmacy practice. These are delivered by skilled teams offering accessible, clinical care in a cost-effective way.
Perpetual struggle
For many independents, it is a perpetual struggle to remain financially stable, leading to reduced hours, a scale-back of services, or losing staff simply to survive.
The value that community pharmacy brings cannot be emphasised enough, but it is often only recognised at breaking point, when a branch closes or when wider healthcare systems become overwhelmed. Every lost pharmacy weakens local capacity, disrupts continuity of care, and depletes community resilience.
The fiscal case for investment is clear: pharmacy is prevention, and prevention is always cheaper than cure. Supporting the sector aligns perfectly with the three shifts outlined in the most recent NHS 10 Year Health Plan.
The demise of LloydsPharmacy and the turmoil surrounding Jhoots should serve as a wake-up call – not just for the profession but for all of us who commission, support and regulate the sector. The fallout from closures of this type has shone a light on an uncomfortable truth: our current regulatory framework needs review and together in the NHS, we must ensure that it aligns with the commercial realities and the future model of modern primary care.
Resetting the framework
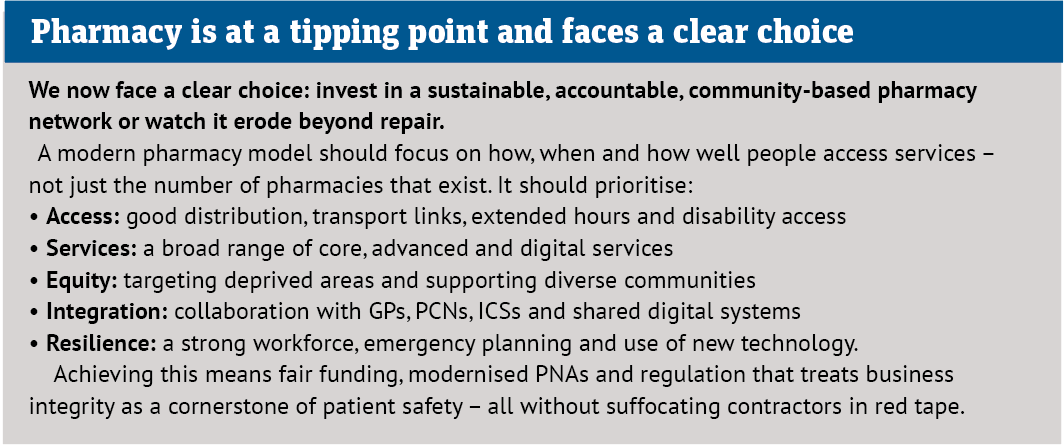
Pharmacy is stuck in a ‘Catch-22’ situation, where it is expected to deliver more services with less funding, while navigating regulatory constraints and medicine shortages.
To unlock its potential, a balance needs to be struck in that we need to free up the sector to do more. We must provide it with the necessary investment and agility to meet changing patient needs, and continue to ensure the highest standard of care is provided. This may require us to look at different approaches to regulation based on the type of model within community pharmacy (retail versus local, NHS versus private).
One starting point is the Pharmaceutical Needs Assessment (PNA). While PNAs are a consistent measure of provision and future need, they no longer reflect the modern community pharmacy landscape and wider primary care access model.
Local authorities are doing a great job within the framework set by PNAs to support community pharmacy access – but PNAs are too static and not always reflective of the changing ways in which patients access services.
The current PNA structure does not reflect the quality, service access and additional capacity community pharmacy can offer.
A reformed, data-driven PNA should be a living tool, responsive to up-to-date information about local health needs, demographics and transport access. It should be capable of influencing commissioning and regulation in a meaningful way, and able to measure the impact a pharmacy can have on the local population.