At first supply
A conversation when the antidepressant is first dispensed can have a powerful effect on whether the person will go on to take the medicine. Privacy is crucial, so an invitation to the consultation room is essential – even for a brief discussion.
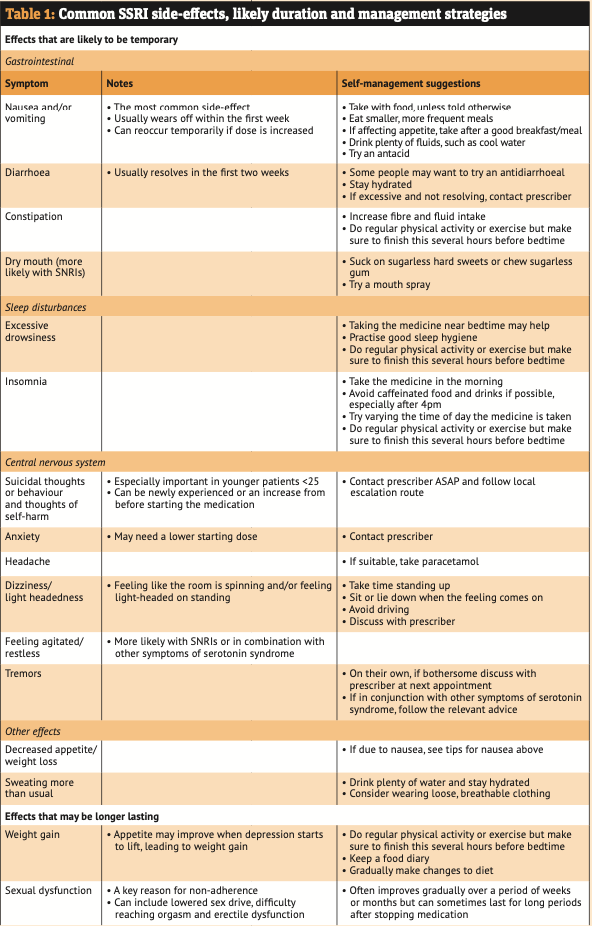
Experiencing side-effects is the most likely reason that someone will stop taking their medicine – and a short conversation makes a difference (see Table 1 for an aide memoire).
When starting treatment, most people will experience at least one side-effect, but most will improve in the early days and weeks. This is why advising on how to manage side-effects through a service like the NMS can have such a big impact.
When the prescription is first dispensed, using the patient information leaflet and pointing out the key sections is a powerful way of focusing the brief conversation.
If the conversation is also to serve as the engagement stage of the NMS, the person should be advised as such and consented.
Possible questions and phrases to use include:
- “I’d like to talk with you about this new medicine so that you know what to expect when you start taking it. You probably have some questions about it and we can talk about how soon it will start working and what to do about any side-effects you get. Is that okay?”
- “What did the GP say to you about what this medicine is for? Have you ever been prescribed an antidepressant in the past or is this the first time?”
- “I’m going to give you some brief information about your medicine. This leaflet has a lot of information and you can use it for reference when you get home”
- “Antidepressants usually take about four to six weeks to work fully and some people’s symptoms start to improve sooner.”
People may use the NHS website as an information source, and you may want to use or adapt these suggested key points from NHS Medicines A-Z in your consultations:
- "These side-effects are usually mild and go away after a couple of weeks”
- “Some people can’t concentrate properly while taking this medicine. It might be best to stop driving, cycling or using machinery for the first few days of treatment until you know how this medicine makes you feel”
- “Do not expect to feel better overnight. Some people feel worse during the first few weeks of treatment before they begin to feel better”
- “It is not common, but some people may have suicidal thoughts or an urge to self-harm when they start taking an antidepressant medicine. Call 999 or go to A&E immediately if you feel like you want to end your life or harm yourself at any time”
- “On the NHS Medicines A-Z, you can look up your antidepressant. There is a section called Common Questions that many people find useful”.
Check if the person is taking other medication, including any OTC medicines, herbal medicines, illicit drugs or alcohol.
Ask these questions non-judgementally and emphasise that it is simply to check for interactions. If they are open to discussion, offer signposting to an appropriate agency/care provider for further support.
At the end of the conversation:
- Ask: “Now that we have had this conversation, are you intending to take your new medicine?” and “how are you feeling about your new medicine?”
- Arrange a consultation for seven to 14 days later or make sure the person knows how to initiate the intervention consultation
- Ask when they next have an appointment with their GP. The early stages of treatment when the mood is lifting is when patients are often at their most vulnerable. It is important to make sure they have support during this time as well as access to a repeat prescription for continuation of treatment.