Clinical picture
Most cases of conjunctivitis are self-limiting and accurate assessment is central to avoiding unnecessary treatment. Viral conjunctivitis is the most common cause overall, particularly
in adults.
Bacterial conjunctivitis accounts for a smaller proportion of cases and is seen more frequently in children. Allergic conjunctivitis is highly prevalent, often seasonal and frequently misinterpreted as infection.
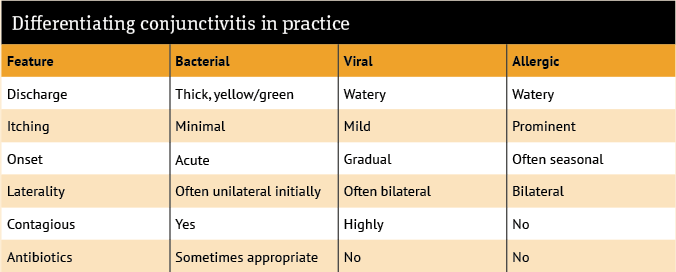
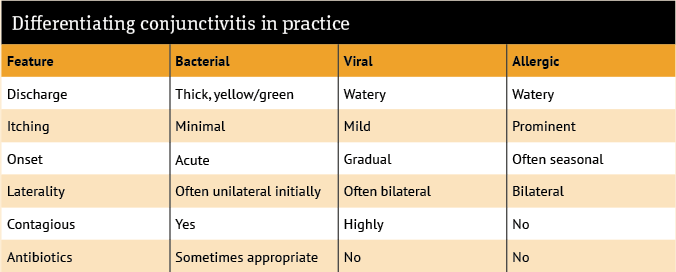
At a pathophysiological level, these conditions differ in ways that translate clearly into recognisable clinical features:
- Bacterial conjunctivitis is commonly associated with Haemophilus influenzae, Streptococcus
pneumoniae and Staphylococcus aureus. It produces a neutrophil-driven inflammatory
response and is typically associated with purulent discharge and lid crusting
- Viral conjunctivitis is most often caused by adenovirus. It presents with watery discharge, redness and irritation, and is highly contagious
- Allergic conjunctivitis is mediated by IgE-driven mast cell activation, resulting in itching, tearing and conjunctival swelling.
Understanding these mechanisms supports more confident and proportionate clinical decision-making in practice.
Effective management begins with a structured consultation. A focused history should explore:
- Onset and duration of symptoms
- Whether one or both eyes are affected
- The nature of any discharge
- The presence and severity of itching.
Symptoms that initially affect one eye more than the other point to an infective cause, as both bacterial and viral conjunctivitis commonly begin unilaterally before spreading. Purulent discharge with eyelids stuck together on waking suggests bacterial infection, whereas watery discharge and a gritty or burning sensation are more typical of viral disease. Where itching dominates, particularly if symptoms are bilateral or seasonal, allergic conjunctivitis should be strongly considered.
Further questioning helps to contextualise the presentation. Recent upper respiratory tract infection or contact with others with conjunctivitis may support an infective cause, while a personal or family history of atopy (such as asthma, eczema or hay fever) increases the likelihood of allergy. Asking whether symptoms are improving, static or worsening also helps to guide advice and follow-up.
Community pharmacists should actively check for features that fall outside uncomplicated conjunctivitis. In particular: pain, photophobia and visual disturbance are not typical and require prompt referral.
Contact lens use deserves specific attention, as it significantly alters risk and lowers the threshold for referral because of the possibility of keratitis (inflammation or infection of the cornea).
In everyday practice, itching remains one of the most helpful distinguishing features. Where the itching is prominent, this strongly suggests allergic conjunctivitis and should prompt consideration of antihistamine or mast cell stabilising treatments for managing the condition, rather than antibiotics.