Analysis

Sliding screens: NHS health screening in crisis?
In Analysis
It’s time to delve deeper into health discussions. Broaden your understanding of a range of pharmacy news and topics through in-depth analysis and insight.Bookmark
Record learning outcomes
Recent reports suggest that the public is confused about the role and value of screening and there is alarming evidence that uptake of national screening initiatives is continuing to fall away each year.

Â
Learning objectives:Â
After reading this feature you should be able to:
- Understand the important role pharmacy has in raising awareness of screening
- Recognise the four hallmark symptoms that can aid in generalised cancer screening
- Appreciate the benefits of providing self-tests for pregnancy, ovulation and fertility, BP, diabetes and intimate women’s health.
Â
There are three national cancer screening programmes active in the UK, looking for breast, bowel and cervical cancer. While mammography for breast cancer and faecal occult blood test (FOBT) for bowel malignancy aim to detect cancer early, Bowel Scope (the latest addition to the English bowel cancer screening armoury) and cervical screening are primarily focused on disease prevention.
However, a recent survey by the National Cancer Research Institute (NCRI) of 1,500 adults shows that the public is failing to grasp the underlying purpose of the national cancer screening programmes, with only a minority aware that screening aims to prevent disease.1
Of those questioned, there was no evidence of understanding or awareness of any difference between the various screening tests.1 Less than a fifth of women knew that the primary goal of cervical screening was preventative and 70 per cent of people surveyed mistakenly thought that flexible sigmoidoscopy was employed largely for early cancer detection.1
“We are not sure why there is uncertainty about what these tests are for,†says Dr Jo Waller, author of the study, “so it is crucial we work with the public to make sure we are providing the best possible information and understand the common questions and misconceptions they may have.â€
The role pharmacy can play in encouraging screening has never been more important. In addition to acting as advocates for the importance of screening, pharmacy teams can also help customers make an informed decision about engagement by outlining the key advantages and explaining the inherent limitations.
“The decision to take part in a screening programme should be an individual choice,†emphasises Dr Waller, “but in order to make a well-informed decision you need a good understanding of what is involved, the balance of benefits and harms, and also why you are being asked to take part in the first place.â€
Â
Location, location, location...
Community pharmacies constitute an “excellent location†from which to offer screening programmes for blood borne viruses (BBV) via dry blood spot testing, according to the Pharmaceutical Services Negotiating Committee.
Pharmacies offer an easy and convenient access point for BBV screening without the need for an appointment and cover the traditional ‘out of hours’ periods of most GPs practices. Customers at high risk of infection with BBVs also tend to be regular users of other allied services provided by community pharmacies, such as needle and syringe programmes and supervised methadone consumption.
PSNC provides a detailed flashcard for use by community pharmacies interested in discussing the BBV screening opportunity with commissioners.9
Timely input
Such an input is timely as latest figures reveal a fall in cervical screening coverage across the UK for the third consecutive year. Data from the Health and Social Care Information Centre indicates a drop in coverage to less than three-quarters (74 per cent) of all women in England invited for screening, with the decrease particularly pronounced in women in the 25-49-year age group (only 71 per cent reported for smear tests).2
A decline in the uptake of testing was also evident among middleaged women, who are invited for cervical cancer screening every five years, rather than every three. In geographical terms, coverage was especially poor in the London area, reaching just over two-thirds of eligible women.
One of the ways in which the Department of Health aims to cut the current cancer death toll in half is by achieving earlier detection of cancer through improved screening. Goals include improving access to screening for all groups and introducing new screening programmes, as recommended by the UK National Screening Committee, where there is evidence they will save lives.
Late-stage diagnosis is recognised to be the single most important reason why cancer survival rates in England continue to lag behind our European counterparts. Approximately 10,000 cancer deaths in England could be avoided every year if cancer survival rates matched the European gold standard.3
Detecting cancer symptoms
Evidence from previous pilot programmes indicates that pharmacies can help drive uptake of NHS breast cancer screening programmes, and improve awareness and encourage early detection of cancers such as skin and bowel cancer.4
Having consistently demonstrated their valuable role in increasing early detection of cancer by raising awareness of the symptoms, community pharmacies are key action areas for Public Health England (PHE)’s general cancer symptom screening campaign – Know4Sure3. Recognising that it is impossible to produce specific campaigns targeting each individual cancer common to the UK, this new initiative is focused on screening for four key symptoms that act as indicators for a constellation of different tumour types:
- Unexplained blood that doesn’t originate from an obvious injury
- An unexplained lump
- Unexplained weight loss that feels significant to the patient
- Any type of unexplained pain that fails to resolve.
Cancer Research UK recommends specific action points for pharmacy to put this generalised cancer screening into every practice:
- Urge any customer complaining of one of the four hallmark cancer symptoms, or using OTC medication to treat them, to visit their GP
- Be confident and, where necessary, give customers ‘permission’ to visit their GP. This can help overcome reluctance to consult based on embarrassment, concerns about time wasting or failure to appreciate the seriousness of symptoms
- Tell the customer to mention to their GP that you (the pharmacist) referred them because their symptoms warranted further investigation
- Encourage pharmacy team members to be confident and follow the normal care protocol, consulting the pharmacist if they feel concerned about a particular patient but are uncomfortable about raising the issue of potential cancer directly
- Make the screening campaign part of everyday community pharmacy practice – e.g. during MURs, OTC sales or in general customer conversations
- Promote the campaign in pharmacy with posters and leaflets.
Â
Self-testing kits and pharmacy
 Pharmacies are a major access point for a range of self-test kits related to fertility/conception. While ovulation home tests pinpoint the rise in luteinising hormone (LH) levels that signals when an egg will be released from the ovary, pregnancy tests rely on detection of human chorionic gonadotrophin (hCG) in the urine.
Pharmacies are a major access point for a range of self-test kits related to fertility/conception. While ovulation home tests pinpoint the rise in luteinising hormone (LH) levels that signals when an egg will be released from the ovary, pregnancy tests rely on detection of human chorionic gonadotrophin (hCG) in the urine.
Other newer fertility tests are also able to measure follicle-stimulating hormone (FSH) levels in the urine. Declining FSH levels are linked to lower oestrogen production and reduced fertility, potentially heralding the onset of the menopause.
Home/portal blood pressure testing kits provide a useful way of measuring and monitoring blood pressure in at-risk patients and those with a confirmed diagnosis of hypertension. The British Hypertension Society provides a list of clinically approved devices. Self-test kits for diabetes are also available that can help to detect high levels of glucose in the bloodstream using a simple finger prick test. Pharmacies can advise on suitable home tests for customers where there is high index of suspicion for type 2 diabetes.
Offering self-tests creates an opportunity to provide several core services (such as targeted MURs or the NMS if a patient is newly prescribed antihypertensives for high BP or requires an oral hypoglycaemic agent after diagnosis of type 2 diabetes) and general advice on a healthy lifestyle, diet and exercise for customers with elevated BP or as a first step in non-pharmacological type 2 diabetes management.
A range of intimate women’s health problems can also be treated with OTC products but optimal management will require accurate diagnosis. Pharmacies can recommend self-test kits for vaginal infection that help to distinguish between conditions like thrush and bacterial vaginosis. This will help steer recommendations on treatment and allow the provision of advice to prevent or reduce recurrence.
Hotspots for screening: HIV and HCV
Following new figures indicating that 18,000 people in the UK are living with HIV but unaware they are infected, PHE has launched the first nationally available HIV screening kit.5 This simple finger prick blood test for people deemed at higher risk of HIV is available to order online. The aim is to improve diagnosis, thereby reducing the risk of unintended transmission and allowing patients to access treatment early to ensure the best possible outcomes.
Currently, around 17 per cent of people with HIV in the UK are estimated to be undiagnosed, including 6,500 men who have sex with men (MSM) and 3,900 men and women from black African communities.5 “Despite national rates of HIV declining, it is still a growing problem within certain communities and levels of HIV testing among high-risk people remain too low,†says Kevin Fenton, national director of health and wellbeing at PHE. “I would encourage all those at higher risk of HIV, such as men who have sex with men or people from black African communities, to seriously consider testing.â€
PHE’s first nationally available free HIV home sampling test follows hot on the heels of the first HIV self-test kits, which went on sale in the UK in April 2015. These self-test kits claim to give results within 15 minutes and provide diagnosis ‘there and then’ with noone other than the patient directly involved. In contrast, the PHE home test kits rely on a blood sample that is sent to an external laboratory for analysis, with results taking around two weeks to be returned.5,6
“HIV testing is key to prevention,†confirms Izzi Seccombe, the Local Government Association’s community wellbeing spokesperson. “Councils now have responsibility for public health and commissioning sexual health services. HIV testing and outreach services are a part of this, whether in GP practices, sexual health clinics or in community settings.â€5
In addition to the issue of undiagnosed HIV among key high-risk populations, there is also evidence to indicate a worrying void in hepatitis C virus (HCV) awareness in the UK, particularly among intravenous drug users (IVDUs).
The latest figures from PHE reveal that almost half (48 per cent) of injecting drug users are unaware they are infected with HCV, despite a relatively high uptake of hepatitis C screening programmes.7 According to Fortune Ncube, consultant epidemiologist and head of PHE’s blood borne virus section, regular HCV screening through engagement with local drug treatment services and primary care remains crucial to safeguard the health of vulnerable drug users.7
Pharmacies are uniquely placed to support improved hepatitis C screening, particularly as higher risk groups (e.g. IVDUs) who would not otherwise engage with health services may be more inclined to visit their local pharmacy. Previous pilot programmes of HCV testing in pharmacies have led to the diagnosis of hepatitis in as many as one in six of all customers tested.
The Hepatitis C Trust currently offers support, including training and the provision of resource materials, to any community pharmacy interested in introducing hepatitis screening services in their local area.8
 PHE has launched the first nationally available HIV screening kit
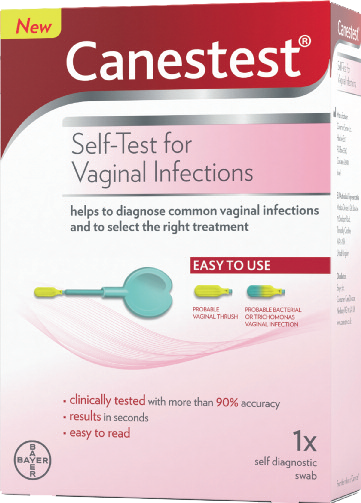 Canestest from Bayer
Canestest from Bayer
Bayer Healthcare has launched Canestest, a selftest that enables women to diagnose common vaginal infections, including thrush and bacterial vaginosis (BV). New research by the company for Self-Care Week shows that nearly half of pharmacy teams think that around half of women avoid seeking help about intimate health concerns and just as many feel that women suffer unnecessarily due to embarrassment. However, 98 per cent of pharmacy staff think that offering women a self-test would help to overcome these issues.
For more information on Canestest products, click here.
Â
Key points
- The public is confused about the role and value of national cancer screening programmes
- Cervical cancer screening coverage in the UK has fallen for the third consecutive year
- Over 18,000 people in the UK are unaware they are infected with HIV
- Up to 50 per cent of injecting drug users are thought to be unknowingly infected with the hepatitis C virus
Â
References
- National Cancer Research Institute (NCRI). ‘Public don’t realise screening can prevent cancer’. Press release: 4 November 2015.
- Prime L. ‘Cervical screening coverage still falling in England’. Press Release: 11 November 2015.
- Cancer Research UK. ‘Know4sure’ campaign: Information for pharmacy teams. Updated October 2014.
- PSNC. Community pharmacy: at the heart of public health.
- Public Heath England (2). Free HIV home sampling launched to increase HIV testing. Press release 18 November 2015
- HIV aware. HIV testing.Â
- Public Health England. ‘Almost half of people who inject drugs unaware they have hepatitis C’. Press release 11 November 2015.Â
- The Hepatitis C Trust. Pharmacy testing.
- Pinnacle Health LLP. Dry Blood Spot Testing for BBV in Community Pharmacies. v1.3 January 2014.Â
