Analysis

PSNC launches five-point plan for pharmacy
In Analysis
It’s time to delve deeper into health discussions. Broaden your understanding of a range of pharmacy news and topics through in-depth analysis and insight.Bookmark
Record learning outcomes
 The national flu scheme is a significant milestone but PSNC’s five-point plan highlights other areas where pharmacy can deliver real value, says director of NHS services Alastair Buxton.
The national flu scheme is a significant milestone but PSNC’s five-point plan highlights other areas where pharmacy can deliver real value, says director of NHS services Alastair Buxton.
So much for the summer holidays! For community pharmacy and, indeed, across a lot of the health service, it feels like life has never been busier. At PSNC attention has, of course, been focused on the recent community pharmacy funding settlement and the new national flu vaccination service, which is set to launch in September.
Milestone
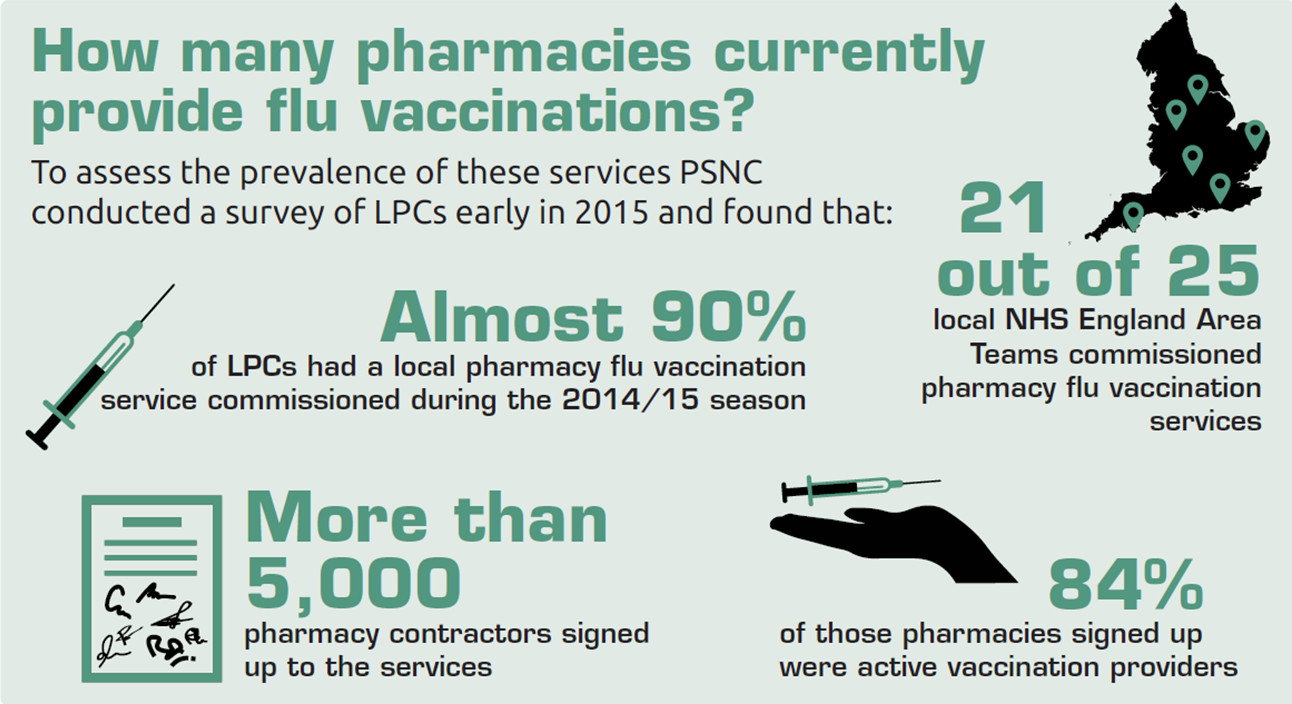
The flu vaccination service is a significant milestone for community pharmacy and really positive news for LPCs, contractors and pharmacy teams alike. A new national service is always an achievement, but this one felt particularly special given the opposition we have faced at so many steps along the way. For example, only last year we heard about doctors trying to block local pharmacy vaccination services – and some are critical of this latest development as well.
The immediate challenge for community pharmacy is to rise above any intra-professional rows and build momentum so we can make this service a real success, helping our patients and our commissioner, NHS England. We must tackle GP negativity where it arises – and PSNC has this month published a range of resources to help LPCs and pharmacy teams to do that – but we should also recognise that we don’t need doctors’ support for this to succeed. Pharmacy teams just need to do what they do best and offer a safe, reliable and high-quality service at the very heart of local communities.
Big changes
While flu may be our top priority – and at PSNC we are working incredibly hard to ensure that the NHS gets everything in place that it needs for the service to launch in September – look beyond pharmacy and it doesn’t take long to get the sense that big changes are afoot in the wider NHS as well. It is now accepted that the health service needs to change radically if it is to survive and remain financially viable, and NHS England is starting to deliver this transformation in a number of different ways.
Across the country, through initiatives like the Vanguard programme and the devolution of the healthcare budget in Manchester, local commissioners are being given budgets with a brief to radically alter models of care, making services more integrated and more consistent for patients. In some cases these initiatives bring with them very real challenges and we are working hard with LPCs in the affected regions to ensure that pharmacy’s interests are protected. We must ensure that the network of community pharmacies in each area is secure and not exposed to local funding shocks or major changes in service.
As is so often the case, along with the risks and uncertainty come some major opportunities. We must capitalise on these. We know that we can be at the heart of a transformed NHS, offering advice, support and a range of services to patients to help them to stay healthy and manage their conditions. We must continue working to convince commissioners and policymakers to enable us to do this in a way that is sustainable and fair to pharmacy businesses.
Plan of action
All of which explains why we are this month publishing a plan of action that we hope will give some more momentum and focus to the development of community pharmacy services. Our pharmacy five-point forward plan (see panel below) sets out five ways in which the NHS could extend pharmacy’s role to enable it to do more in the evolving NHS world.
If the plan were implemented, we believe it would cement pharmacy’s position in healthcare, as well as improving the experience of patients and delivering value for the NHS. You can find the plan at PSNC: 5 point plan
Â
PSNC's 5-point plan for pharmacy
1. Give patients easier access to urgent medication
Commission an urgent supply service so community pharmacists can supply routine NHS prescription medication at weekends and out-of-hours if patients run out.
2. Offer people advice at their own convenience, using pharmacy as a first port of call
Use community pharmacists to advise people with symptoms, offering treatment or referral as needed.
3. Care for frail and older people
Community pharmacists can provide support to frail and older people and their carers at their homes if necessary. This ensures they are using medicines properly and safely, particularly after hospital discharge.
4. Support people to manage their long-term conditions more effectively
Community pharmacists should support and monitor people with simple hypertension and asthma to help them to manage their own health.
5. Help identify people with undiagnosed respiratory disease
Community pharmacists should provide risk assessments for people potentially at risk of having or developing COPD, followed by advice and stop smoking support or referral.
All to play for
This is a time of huge change within the health service and pharmacy absolutely must take every chance to bolster its position within the evolving systems. We can start now with flu vaccinations, showing commissioners just how much of a difference we can make. As this service has shown us, there will be obstacles along the way and some people will always be unhappy to see pharmacy succeed – but we can and will get over that. It is most definitely all to play for.
Web exclusive: Q&A with Sue Sharpe, PSNC chief executive
 Why did negotiations over a national minor ailments scheme break down?
Why did negotiations over a national minor ailments scheme break down?
We were not able to agree on the details and funding for the service. For PSNC and contractors, as NHS financial pressures continue, it is essential that we do not negotiate an under-funded service.
The proposal that we advocate uses community pharmacists’ professional skills to offer advice to patients, together with medication if needed. This advisory service is quite different in time, resource and therefore cost from schemes that primarily use pharmacies to supply medicines, such as head lice lotion. I think there was a failure in NHS England to grasp the differentiation and perhaps really consider how this could relieve pressure on GP resources.
It is a massive missed opportunity for them. Our understanding had been that the benefits to be realised were well understood in NHS England, but the eventual disappointing decision means we need to set out the case, and persuade NHS England of the impact that a community pharmacy minor ailments advice service could have in reducing demand for GP and urgent care services.
Is it a realistic expectation to think that agreement will be reached on a minor ailments scheme in time for next year’s settlement?
I don’t know. For us it is essential to get the service specification right and to agree proper funding. If the NHS focuses on the cost rather than on the cost savings to the system and the taxpayer, then we may not be able to achieve our aim. This would be very frustrating – this service is probably the biggest contribution that pharmacy
could make towards achieving the system changes the NHS needs, and it could be implemented very quickly.
I worry that there is still an institutional myopia in parts of NHS England that inhibits clear vision of the potential of community pharmacy services.
How do you respond to claims that the £2.8bn funding settlement for 2015/16 simply represents “more for less†when compared to the 3.3 per cent annual increase in prescription items?
The NHS publicly set out its demands for a minimum 4 per cent efficiencies across the NHS. A part of this efficiency demand on community pharmacy was met by dealing with the increased prescription volume. This is difficult for contractors to manage, but I do not know of any part of the NHS that is not facing acute pressures from the need to reduce cost growth. So it is correct to say that this is more work for the same funding.
What would you say to contractors in advance of the national pharmacy flu vaccination service starting next month?
Community pharmacy flu vaccination services have been an immense success.
The widespread adoption of locally commissioned NHS and private vaccinations represents a significant extension of the pharmacist’s role. I believe it has a positive effect on peoples’ perception of community pharmacists' professional status.
The future health of community pharmacy is, unarguably, dependent on its ability to provide a wide range of services for patients – in public health (as with the flu jabs) and in supporting patients. My message to contractors: make the service a great success in your pharmacy. Prove to patients and the NHS that when patients have a choice, they are happy to trust the professionalism, and value the convenience of, community pharmacy.
It will be good for the pharmacy. This is a powerful contribution that every pharmacy can make to help us secure more properly funded services in the future.
Are you confident that any potential vaccine supply problems can be overcome in time for the start of the service?
No. The delays in finalising the settlement and late announcement may give rise to supply problems this year, but we will be better able to predict and manage demand for the winter 2016 season.
Why have you chosen now to draw up a five-point plan for PSNC and what do you hope to achieve by this?
We want to state very clearly and loudly how community pharmacy can step up its contribution to primary care, in a short timescale. Our objective is principally to get ministers and NHS England to address these points in our next round of negotiations, and to focus on the opportunities on offer. The five points are all in PSNC’s vision, but following the disappointment with the minor ailments advice service we decided we needed to articulate very clearly and specifically what community pharmacy service expansion can do and the value it brings to patients and the NHS.
How does PSNC feel about the proposed funding reforms suggested by the Royal Pharmaceutical Society in its joint consultation with the National Association of Primary Care?
We have made our concerns about the funding elements of the RPS and NAPC proposals public. A national contract is protective armour, not a straightjacket. There is nothing in the RPS service ambitions that is incompatible with maintaining a strong core national contract.
Funding systems and business viability issues are, of course, not parts of the role or expertise of the RPS, and I think those parts of the proposals suffered from a lack of rigorous scrutiny of the risk to the foundations of the community pharmacy network. My greatest fear is that the immense value of the investment and service community pharmacy provides will be put at risk by laudable aspirations to develop pharmacists' role.
There is much in the proposals that we support, and I really hope the RPS and NAPC will reflect on our concerns and amend their proposals. We will of course be submitting a full response to the consultation and I hope others will do so too. At its worst, adoption of the proposals would lead to a poorer service to patients and the effective end of independent professional community pharmacy.
We know that we can be at the heart of a transformed NHS
