Allergy management: Shock tactics
In Clinical
Follow this topic
Bookmark
Record learning outcomes

As the number of allergy sufferers in the UK continues to rise, so too does the rate of anaphylaxis €“ yet public awareness of this severe reaction is still startlingly low.
Learning objectives
After reading this feature you should be able to:
- Respond in the event of a customer experiencing an anaphylactic shock
- Raise awareness of the symptoms of anaphylaxis and the impact on the daily lives of sufferers
- Support patients who have been prescribed an adrenaline auto-injector (AAI) to use it with confidence
Latest NHS statistics reveal that hospital admissions for allergic reactions have soared in recent years to reach more than 20,000 cases annually. Over 60 per cent of allergy-related hospital admissions are for anaphylaxis €“ the most severe, often lifethreatening form of allergic reaction. Prescriptions for adrenaline auto-injectors (AAIs), administered during anaphylaxis, have also risen.
Prescribing information for the 12 months to February 2014 shows that 353 emergency adrenalin products were prescribed per 100,000 head of the population, equivalent to one item per 283 people. However, while prevalence of anaphylaxis is on the rise, research by Allergy UK has highlighted a worrying lack of public knowledge and understanding about the condition, while millions of allergy sufferers are living in daily fear of experiencing a severe reaction.
The 'old friends mechanism'
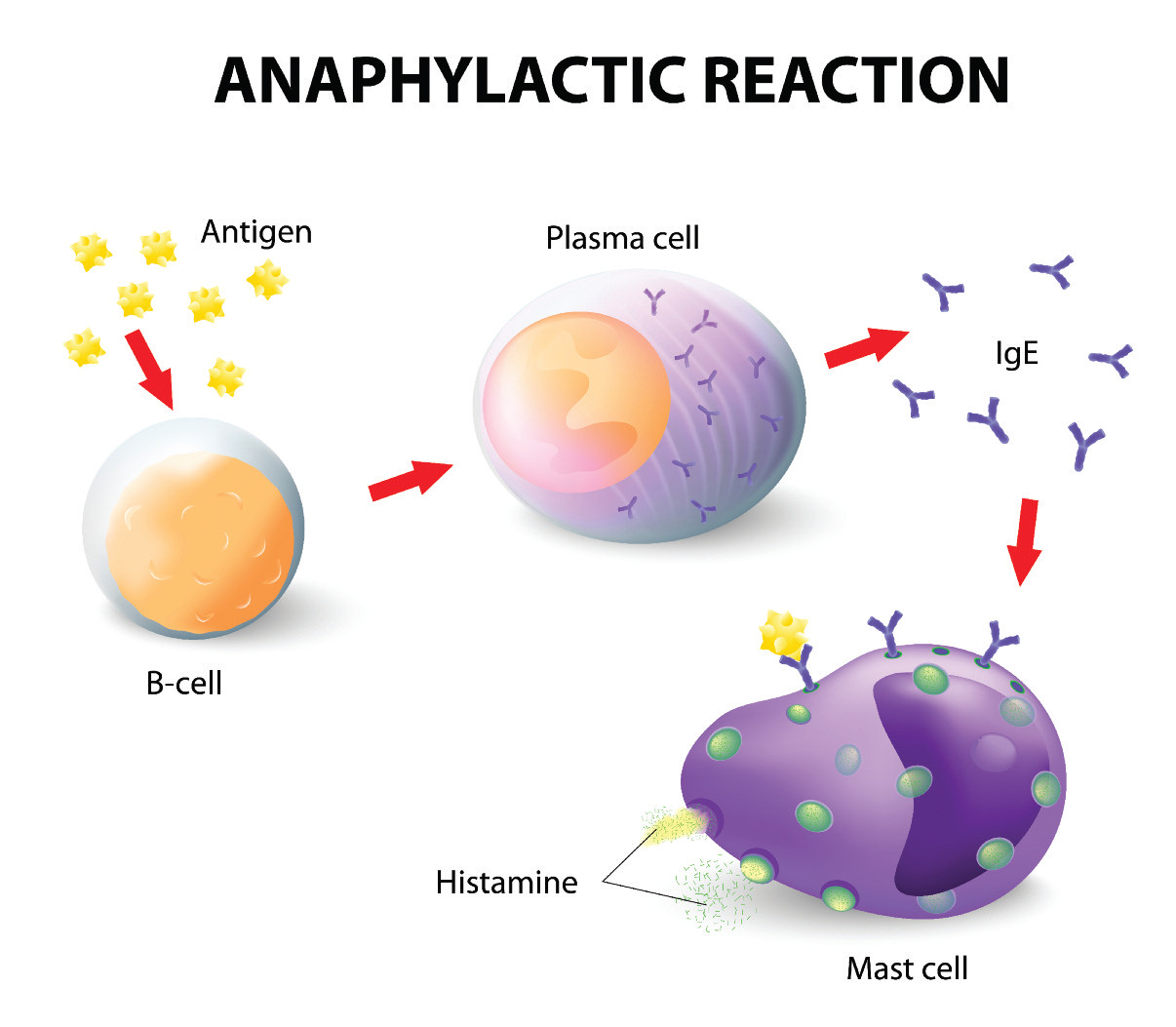
As with any allergy, an anaphylactic shock occurs when the immune system reacts inappropriately to the presence of a substance that it wrongly perceives to be a threat. In the case of anaphylaxis, the reaction is systemic, involving more than one system, such as the skin, gut, circulation and respiratory tract. It usually occurs within minutes, but sometimes the time lapse between exposure to the allergen and a reaction can be hours.
According to Allergy UK and the Anaphylaxis Campaign, anaphylaxis incidence has risen in line with the dramatic increase in allergic diseases, such as allergic rhinitis, food allergy and eczema. The most accepted theory behind the rise in allergy is known as the 'old friends mechanism', whereby decreased interaction with immuno-regulating micro-organisms impairs the healthy development of the immune system.
€Due to factors like the rise in Caesarean sections, vaccination, the decline in breastfeeding, and increased exposure to pesticides and disinfectants, our environment has changed and we are not as exposed to the same degree of microdiversity as we were in the past,€ explains Moira Austen, helpline and information manager at the Anaphylaxis Campaign.
€Another factor may be that allergy is more frequently diagnosed and recognised that it was previously.€ Allergists are moving away from talking about the 'hygiene hypothesis' in favour of the 'old friends mechanism' to avoid confusion over the importance of basic hygiene.
€It is still important to be hygienic in terms of washing hands in food preparation or after using the toilet; it is just not necessary to wipe off every bit of mud or wash your hands 20 times a day,€ says Maureen Jenkins, chief executive of Allergy UK.
The commonest allergens that trigger anaphylaxis include medicines, particularly antibiotics, insect venom and certain foods, particularly peanuts, tree nuts, egg, soya, wheat, shellfish, fish, sesame and some fruits. For babies, milk can be a trigger. Intensive exercise can also bring on an anaphylactic shock while, in some cases, the trigger cannot be identified.
Any individual can develop a severe allergy at any time, but those with a genetic predisposition to allergy (atopy), particularly people with asthma, are at increased risk. If a significant reaction has occurred in response to a small dose of a substance or following skin contact, this could be a sign that a greater dose may trigger a severe reaction.
While it is impossible to prevent children developing anaphylaxis, the advice for pregnant women is to eat as wide a variety of foods as possible and not to avoid anything unless they are allergic themselves. €Avoiding nuts, for example, is not a good idea,€ says Maureen Jenkins.
Responding to symptoms
Recognising the symptoms is essential to ensure that an individual experiencing an anaphylactic reaction receives the necessary treatment. However, a recent survey by Allergy UK revealed that nearly half (44 per cent) of people in the UK have no idea what anaphylaxis is. As anaphylaxis is a systemic reaction it can cause a wide range of symptoms, varying in severity, including:
- Generalised flushing of the skin
- Nettle rash (hives) anywhere on the body
- Swelling of the throat and mouth
- Difficulty in swallowing or speaking
- Alterations in heart rate
- Severe asthma
- Abdominal pain
- Nausea and vomiting
- Sudden feeling of weakness (drop in blood pressure)
- A sense of impending doom or helplessness
- Collapse and unconsciousness.
The only treatment for anaphylaxis is an intramuscular injection of adrenalin, which is usually delivered via an AAI into the thigh. After injecting, the syringe should be held in place for five to 10 seconds. Injections can be given through clothing. Following treatment, the advice is to get the patient to lie down with their feet raised and call an ambulance, stating anaphylaxis, as delayed symptoms may occur.
Most people who have experienced an anaphylactic reaction will be prescribed an AAI and, under an exemption in the Medicines Act, anyone is able to administer adrenalin if they suspect that someone is having an anaphylactic shock.
While the treatment of anaphylaxis is relatively simple, 68 per cent of people surveyed by Allergy UK feel €scared, hesitant or anxious€ at the thought of having to administer an adrenalin autoinjector, while 66 per cent admit that they have no idea how to use an emergency adrenalin product. Young people aged 18-24 years are the least 'allergy aware', with three-quarters not knowing how to help someone having an anaphylactic reaction.
€Lots of people are worried about giving adrenalin. If they administer it incorrectly it will cause palpitations and a rapid pulse, which will gradually subside, but if they don't act then the consequences can be very sad,€ says Maureen Jenkins. €It is important to add that people do not have to be wheezing to be having an anaphylactic reaction; they may just be struggling to talk,€ she adds.
The survey also highlighted widespread confusion between the symptoms of anaphylaxis and those of a heart attack or stroke.
One in four people mistake facial weakness as a symptom of a severe allergic reaction and 15 per cent wrongly cited pain down the arm as a sign of anaphylaxis. Allergy UK is calling on people to familiarise themselves with symptoms by using the FEAR pneumonic:
- Face - is their face/are their lips swollen? Have they gone pale? Are they lightheaded?
- Eyes - is there a look of fear in their eyes? Are they red, watery and puffy?
- Airways - are they wheezing/uncontrollably coughing? Do they have a shortness of breath? Are they unable to talk? Are they making a strange sound?
- Rash - is there a red, raised, itchy rash anywhere on their body, especially their face or neck?
Key facts
- There are 20,000 hospital admissions and 20 deaths due to anaphylaxis in the UK every year
- Nearly half of severe allergy sufferers live in daily fear of anaphylaxis
- Most Britons do not know how to recognise or respond to anaphylactic shock
Living in fear
Allergy UK is concerned that this lack of life-saving knowledge could be endangering the lives of millions of severe allergy sufferers in the UK. Every year at least 20 people die from anaphylaxis, and nearly half of the 2,000 anaphylactic sufferers surveyed by the charity reported living in daily fear of experiencing a reaction. For instance, ninety-two per cent said they were concerned about eating out, while 82 per cent worry about going on holiday.
€Sufferers are often terrified to eat out at restaurants or other people's homes,€ says Maureen Jenkins. €It can affect them emotionally and socially and impact on their relationships.€ The impact of anaphylaxis on daily life depends on the individual and the allergen, says Moira Austen.
€People with wasp venom allergy may feel secure during the winter but will have to be very careful in summer, covering up their arms and not going barefoot, for example,€ she says. €But for people with food allergies, it can affect their whole lives and be particularly challenging for parents. Some people avoid eating out or don't travel abroad.€
Both Allergy UK and the Anaphylaxis Campaign are concerned that severe allergy is often not taken seriously enough and believe there should be more education about the reality of anaphylaxis in schools. One in four sufferers (26 per cent) have been teased or bullied about their condition and one in three (32 per cent) say that they lack self-confidence.
€Parents may not understand why they can't send their kids to school with peanut butter sandwiches if a classmate has a severe peanut allergy. If you don't have a close family member with anaphylaxis it can be hard to appreciate the severity of the condition,€ says Moira Austen.
Pharmacy action
The Anaphylaxis Campaign and Allergy UK believe that pharmacists have a responsibility to help save lives by raising awareness of severe allergies and ensuring they can respond if they suspect a customer is having an anaphylactic reaction.
Community pharmacists are required to learn how to respond to anaphylaxis during their pre-registration year but there is no requirement to ensure that they keep this knowledge up-to-date, although pharmacists must undergo the training in order to provide flu vaccination services. In Scotland, there is an ongoing initiative to ensure that every pharmacist has a general AAI available for customers if it is required in an emergency.
Maureen Jenkins also stresses the need for pharmacists to ensure that patients who are prescribed an AAI feel confident about using it. She advises pharmacists to keep dummy AAIs for each of the three emergency adrenalin products available so they can ensure they are familiar with the different injection methods and be ready to demonstrate how they work whenever a patient presents with a prescription for an AAI.
€Customers may also need reminding how to use them, or need training if they are given a different device or brand to the one they normally have,€ adds Moira Austen. €Pharmacists should also be prepared to answer questions and direct customers to reliable resources of support and information,€ she says.
Allergy toolkit
The grass hayfever season may be nearly over, but shrub and weed pollen will be in the atmosphere until September, while mould and spore pollen will bring problems for many allergic rhinitis sufferers during the autumn. In addition, whenever there is hot weather, customers will continue to present with seasonal allergies e.g. insect bites and stings, nettle rash and polymorphic light eruption. It is essential that pharmacies are ready with the right treatments to help allergy sufferers manage symptoms all-year-round.
Antihistamines
Available in tablet, cream and spray formats, antihistamines can relieve the symptoms of various allergies, including allergic rhinitis, insect bites and stings, and skin reactions. Second and third generation antihistamines, such as loratadine and cetirizine, should be recommended over first generation antihistamines (e.g. diphenhydramine and chlorphenamine) as the latter may cause drowsiness. However, first generation antihistamines may be beneficial at night if allergy symptoms are causing sleep disturbance.
Barrier products
Barrier products in the form of gels or balms aim to prevent hay fever symptoms by stopping airborne allergens from entering the respiratory tract through the nose. Some products claim to neutralise or inactivate allergens as well as forming a protective film over the nasal cavity. These drug-free options are non-drowsy, suitable for children and pregnant women, and can be used in conjunction with drug treatment.
Corticosteroids
Nasal corticosteroids help to control hay fever symptoms on a long-term basis for patients suffering moderate to severe symptoms. Customers should begin using these products in advance of the typical onset of symptoms as they can take up to two weeks to work. A combination product containing an antihistamine and a corticosteroid may benefit customers who struggle to take lots of different products. Topical steroids can help relieve skin reactions.
Crotamiton
Crotamiton cream or lotion is a general antipruritic, which can be used to relieve itching or skin irritation due to skin conditions such as allergic rashes, bites and stings, sunburn, eczema, dermatitis, nettle rash, chickenpox and heat rashes.
Decongestants
Allergy sufferers may be unaware that they can use oral or nasal decongestant sprays to relieve nasal congestion associated with allergic rhinitis. These products work rapidly and can be taken in combination with antihistamines to relieve other symptoms but topical sprays must only be used for a period of five to seven days to avoid rebound congestion.
Sodium cromoglicate
The symptoms of allergic conjunctivitis (e.g. red, itchy or watery eyes) due to contact with pollen, dust mites, pet dander or cosmetics, can be effectively managed with sodium cromoglicate eye drops. Contact lenses should be removed before applying the drops.
Sunscreen
Polymorphic light eruption or sun sensitivity can be triggered by UVA as well as UVB rays, so it is essential that susceptible individuals apply a high sun protection factor cream that offers protection against both forms of UV light.
Key contacts
- Allergy UK: www.allergyuk.org Helpline: 01322 619 898
- The Anaphylaxis Campaign: www.anaphylaxis.org.uk helpline: 01252 542 029
