Clinical

IBS: Spell it out
In Clinical
Let’s get clinical. Follow the links below to find out more about the latest clinical insight in community pharmacy.Bookmark
Record learning outcomes
With research showing that one-third of patients don’t believe healthcare professionals take irritable bowel syndrome seriously enough, the need for better communication between care providers and patients to improve outcomes is clear

Irritable bowel syndrome IBS) can be mentally and physically draining, leading to time off work and the avoidance of social occasions. Research published in the United European Gastroenterology (UEG) Journal found that one in 10 IBS patients who experience diarrhoea as their predominant symptom even suffer from suicidal thoughts when their condition is at its worst.
A quarter of patients reported that IBS stops them from enjoying life, while over a third reported that they constantly worry about whether and when their IBS symptoms will return. One in five said that IBS had negatively affected their working life, with anxiety and depression the commonest co-morbidities.
While there are no ‘quick fix solutions’ for IBS, most people after their initial diagnosis can manage their symptoms with dietary and lifestyle changes and OTC medicines.
IBS: what is it?
- Irritable bowel syndrome (IBS) is a chronic digestive disorder affecting up to one in five people in the UK (mainly adults between 20 and 30 years of age)
- It is twice as common in women than in men
- The main symptoms are abdominal pain, bloating and a change in bowel habits (diarrhoea, constipation or alternating, between the two)
- It can also cause other non gut-related symptoms, such as lack of sleep, fatigue, bladder problems and backache.
Getting a diagnosis
According to NICE guidelines on IBS in adults (updated in April 2017), symptoms may overlap with other gastrointestinal disorders, such as inflammatory bowel disease or coeliac disease, making the condition difficult to diagnose. Anyone with IBS symptoms should consult their GP to rule out anything more serious before they try to treat their symptoms themselves (or with the help of a pharmacist).
IBS may be considered by a GP if an adult has recurrent abdominal pain or discomfort on at least one day a week for at least six months. Symptoms ease when the bowels are opened and may be associated with a change in stool frequency and/or form (i.e. diarrhoea, constipation, or both). Sufferers will also have at least two of the following four symptoms:
- A change in how they empty their bowels (straining, urgency, incomplete evacuation)
- Abdominal bloating (especially in women), tension or hardness
- Symptoms made worse by eating
- Passing mucus from the rectum.
IBS is a functional disorder – affecting how the gut works but not causing any noticeable changes in the bowel tissue. The exact cause is not known precisely, but the condition may be due to a combination of gut hypersensitivity, microbial imbalance in the gut and defective pain pathways (see panel below). “The diagnosis of IBS is not always clear cut, as there is no single diagnostic test to confirm a person has it,” says Dr Sarah Brewer, GP, medical nutritionist and author.
“Doctors therefore need to rule out other conditions that can cause similar symptoms and to exclude cancer of the bowel, ovaries or other structures. At the same time, it is important to avoid a battery of tests in people who don’t have ‘red flag’ symptoms, such as a family history of bowel or ovarian cancer, weight loss or blood in the motions.
“New guidelines suggest that people who develop symptoms for the first time over the age of 50 years should be offered a screening colonoscopy, but each case is different and requires thoughtful questioning and physical examination, with appropriate tests and follow-up. That follow-up is important – customers shouldn’t be afraid to keep going back to their doctor if their symptoms persist, are worsening or changing.”
Trigger identification
IBS can’t be ‘cured’, so the aim of treatment is to ease the symptoms and reduce the frequency of flare-ups. Once diagnosed, IBS patients should keep a symptom diary to try to establish their main triggers, assessing their sleeping habits, eating habits, exercise levels and intake of certain foods or drinks (e.g. caffeine, fat, alcohol and/or gas-producing foods such as cabbage).
“Pharmacists may be able to offer timely intervention for many patients with IBS,” says Dr Simon Smale, consultant gastroenterologist in Manchester and spokesperson for The IBS Network charity (theibsnetwork.org). “A fairly simple review of a person’s lifestyle may identify modifiable factors.”
Lifestyle and dietary advice needs to be tailored to the individual patient. Some people find their symptoms improve if they take more regular exercise, eat regular meals, watch what they eat and drink, and/or manage their stress levels (see panel on IBS self-management tips).
“A recent study from a group in Melbourne showed that yoga was comparable to a low FODMAP diet in providing relief from IBS symptoms,” says Bridgette Wilson, specialist gastroenterology dietitian at London Dietitians Ltd and Guy’s and St Thomas’ NHS Foundation Trust. “There is certainly a psychological component to IBS and therefore it makes sense that stress-relieving exercise and increased mindfulness or meditation may be helpful.”
Some pharmacy customers may find that they need to review their fibre intake, eating more soluble fibre (e.g. oats) and less insoluble fibre (e.g. bran). “Fibre helps to get things moving, although it can make symptoms worse in some people,” says Sarah Brewer.
“As well as eating more fruit and veg, beans, salads, nuts and seeds (e.g. chia, flaxseed), supplements such as psyllium will ‘feed’ bowel bacteria and absorb water to add bulk. While this approach usually works, it can take up to four weeks to notice the benefit. Fibre intake shouldn’t be increased too quickly as this may lead to bloating and discomfort. Fluid intake needs to be increased so the fibre doesn’t dry out and make symptoms worse.”
Pharmacists are ideally placed to support any behavioural changes, as well as recommend evidence-based self-help information. “Patients can be directed to useful sources of information such as the NHS website and gut health experts such as Gut UK [the British Society of Gastroenterology charity, formerly Core] and the IBS Network,” says Linda Thomas, science consultant for PrecisionBiotics and organiser for the Gut Microbiota for Health expert panel of the British Society of Gastroenterology.
“The British Dietetic Association also has useful fact sheets on IBS and diet, as well as information on fibre, fruit and vegetables.”

Gut feelings…
Until recently, IBS was considered to be purely a disorder of bowel function but it is now referred to as a disorder of gut-brain interaction, with the involvement of the gut microbiota/microbiome (altered or unhealthy levels of bacteria in the gut). The gut microbiota is a hot topic of research, and it is hoped that targeting the gut-brain axis will lead to new IBS treatments in the future, particularly for stress-related symptoms.
“The brain and the gut have an intrinsic link,” says Dr Sean Bennet, postdoctoral research fellow at Queen’s University, Ontario, Canada. “Someone who is nervous may have the feeling of butterflies in their stomach. In patients with IBS, these butterflies might be a little more aggressive and a bout of anxiety could lead to a rush to the bathroom. Similarly, levels of depression might lead to an improper functioning of the gut, which in turn potentially leads to the symptoms used to diagnose IBS.”
Research suggests that some gut bacteria produce neuroactive metabolites capable of affecting a person’s mood. The gut is involved in the production of more than 90 per cent of the serotonin found in the body. “We now understand that not only do messages travelling from the gut – so-called gut feelings – have an impact on our emotional wellbeing, so too does our environment impact on how we perceive what’s happening and how our guts behave,” says Dr Simon Smale, consultant gastroenterologist in Manchester and spokesperson for the IBS Network.
“We are beginning to understand how early life, or even the lives of our parents, may impact our microbiome. The childhood microbiome may then impact on the development of both the central and enteric nervous systems, which has subsequent effects on our immune, nervous and psychological health later in life. All of these complex interactions have important implications for the development of IBS in adulthood.
Pharmacy management
Mark Cox, consultant gastroenterologist at Spire Little Acton and Spire Parkway Hospitals, says it is important that pharmacists reassure IBS patients about their symptoms once they have been diagnosed. “The initial pharmacy management is usually reassurance that there is nothing sinister going on and that the symptoms are likely to resolve with time,” he says.
“Pharmacists, of course, can offer advice about OTC medicines. They should, however, suggest that if customers are no better after a short period of time and their symptoms don’t settle relatively quickly, they should see their GP.”
Over-the-counter medicines for IBS include laxatives if patients suffer from constipation (but not lactulose as this can cause bloating), loperamide for diarrhoea and/or antispasmodics such as mebeverine hydrochloride or peppermint oil. “Where appropriate, pharmacists may be able to offer symptom-targeted interventions such as antispasmodics, antidiarrhoeals or aperients [for constipation] to address particular complaints,” says Simon Smale.
“Sometimes these products can be very helpful, but controlled trials often demonstrate a high – 30 per cent or more – placebo response and even the best medicines are only effective for a proportion of patients.”
Some IBS patients find that probiotics (such as combinations of Lactobacillus and Bifidobacteria added to yoghurts or found in supplements) help to reduce their symptom severity. According to NICE guidance, patients should take a probiotic product for at least four weeks, at a dose recommended by the manufacturer, noting any changes in their symptoms.
“Probiotics may work in a more fundamental way in the gut than OTC medicines, because probiotics are targeting the gut microbiota, which may be the root of the problem,” says Linda Thomas. “In contrast, many OTC medicines target one or more symptoms. Not all probiotics have the same effects, however, so it is important that patients are guided to choosing a goodquality probiotic supported by appropriate scientific evidence relevant to IBS.”
Red flags
IBS can be mistaken for other more serious gastrointestinal disorders, so it is important that pharmacy customers (including those already diagnosed with IBS) are referred to their GP if they experience any of the following symptoms:
- Weight loss for no known reason
- Bleeding from the anus or bloody stools
- A hard lump or swelling in the abdomen
- Shortness of breath, noticeable heartbeats (palpitations) and pale skin.
Specialist diets
Some people find that one specific food triggers their IBS symptoms and, depending on the food, they may be able to cut it out of their diet or at least reduce consumption. NICE guidance stresses, however, that customers planning a restricted diet should seek advice from a dietitian to make sure they are still obtaining enough essential nutrients.
The low FODMAP diet is a popular second-line management approach that some people find very effective. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are a collection of poorly absorbed carbohydrates that are found in a variety of fruits and vegetables and also in milk and wheat. IBS symptoms, such as bloating, wind and pain, can be triggered by the breakdown of these foods by gut bacteria. FODMAPs can also draw water into the bowel, causing diarrhoea.
The low FODMAP diet has been studied in several clinical trials in patients with IBS. “Results show a better response to low FODMAP diets than traditional diets,” says Professor Giovanna Barbara, associate professor at the department of medical and surgical sciences at the University of Bologna, and spokesperson for the UEG. “The available data is still limited by the low number of patients studied and the difficulties in the design of foodrelated trials in IBS. In addition, these diets should be used with caution as they may determine nutritional imbalances, including reduction of iron and calcium levels.”
If IBS patients are eating large quantities of high FODMAP foods (e.g. onions, garlic, brassicas or stoned fruit), a dietitian may suggest reducing their intake to see if this improves their symptoms, rather than following a strict low FODMAP diet. A low FODMAP diet doesn’t work for everyone with IBS and needs to be well planned. In the long-term, it can reduce the biodiversity of the gut microbiota, so after a couple of months low FODMAP foods need to be gradually reintroduced in a structured way.
“It can be a complicated diet to stick with,” says Bridgette Wilson. “It is important to maintain a good fibre intake while following the diet, as research has shown that, compared to baseline, patients following a low FODMAP diet reduce their fibre intake.
“A recent systematic review of the efficacy of low FODMAP diets suggests that it may be less effective for patients with constipation-predominant IBS, although this isn’t always clearcut. A dietitian can help a patient to decide, based on their symptom profile, if a low FODMAP diet or a partial low FODMAP diet may be more appropriate to their needs.”
IBS self-management tips
NICE guidance recommends the following lifestyle tips for IBS patients:
- Avoid obvious causes of stress and have more relaxation time
- Take some regular exercise
- Don’t rush mealtimes
- Stop smoking
- Avoid missing meals or leaving long gaps between eating
- Drink at least eight cups (around two litres) of fluid every day, especially water or other non-caffeinated drinks (such as herbal teas)
- Restrict caffeinated tea and coffee to three cups a day
- Reduce intake of alcohol and soft drinks
- Limit fresh fruit to three portions per day (a portion should be around 80g)
- Avoid sorbitol, an artificial sweetener found in sugar-free sweets, drinks and in some diabetic and slimming products, if the person has diarrhoea
- Eat 30g of fibre a day (although too much fibre can trigger symptoms in some IBS patients).
Prescribed treatments
If dietary and lifestyle changes aren’t working for a pharmacy customer, they should be referred back to their GP for prescribed treatments, such as linaclotide, which is licensed for the treatment of moderate to severe IBS associated with constipation.
“GPs may well try alternative antispasmodics and some of the more modern gut-specific drugs,” says Mark Cox. “They may also feel that a low dose tricyclic antidepressant could be helpful. They are often used as pain modulators as well as for their anxiolytic and antidepressant effects.”
If IBS patients haven’t responded to pharmacological treatments after 12 months, they can be referred for psychological therapies by their GP. According to NICE guidance, cognitive behavioural therapy (CBT), hypnotherapy (specifically aimed at gut health) and psychological therapy are thought to be useful in helping people with IBS to cope, even those with moderate to severe symptoms, but it is not yet clear whether they should be first-line approaches.
Customers may also benefit from trying CBT, mindfulness or general relaxation therapies themselves (with the help of books, apps, websites or local therapists) to see if their symptoms improve. Pharmacy teams can signpost where appropriate.
“There is evidence to support CBT for IBS symptoms and [improving] quality of life,” says Linda Thomas. “However, efficacy may depend on whether stress is the main trigger for IBS in a particular patient. One problem can be the limited availability of appropriate resources and expertise. Patients may find it difficult to be referred or find a therapist with the necessary background.”
Coeliac disease: diagnoses up but testing slows
Recent research for Coeliac UK shows diagnoses of coeliac disease rose by a quarter from 24 to 30 per cent between 2011 and 2015 but the rate of diagnosis is now slowing significantly. As a result, around half a million people in the UK are still living with undiagnosed coeliac disease.
The research, commissioned from the University of Nottingham, also highlighted that one in four adults over 18 years diagnosed with coeliac disease had previously been misdiagnosed with irritable bowel syndrome (IBS). The NICE guidelines for coeliac disease and IBS recommend that anyone presenting with IBS symptoms should be screened first for coeliac disease. “It is fantastic that the research shows around 45,000 people were diagnosed between 2011 and 2015 but with half a million people in the UK still without a diagnosis we’ve got a long way to go,” says Sarah Sleet, chief executive of Coeliac UK.
“The fact that testing for the condition is slowing and nothing has changed in people being diagnosed with IBS before being tested for coeliac disease suggests the NHS is failing to address the mountain of under-diagnoses. We know this is even more urgent today as recent research is uncovering some symptoms of coeliac disease, specifically neurological ones, that cannot be reversed without an early diagnosis.”
On average, it takes 13 years for a person with coeliac disease to be diagnosed, Coeliac disease is a serious autoimmune condition caused by a reaction to gluten. It is estimated to affect one in 100 people. “The blood test for coeliac disease is relatively quick and cheap and we urge anyone that has ongoing symptoms to visit their GP and request to be screened for coeliac disease,” says Sarah Sleet.
“Next year we will be targeting doctors to encourage them to consider if their patients could be suffering with undiagnosed coeliac disease or have been misdiagnosed with IBS, and ensure they do not remove gluten from their diet prior to testing as this could lead to a false negative result.”

 According to NICE guidelines on IBS in adults (updated in April 2017), symptoms may overlap with other gastrointestinal disorders, such as inflammatory bowel disease or coeliac disease, making the condition difficult to diagnose. Anyone with IBS symptoms should consult their GP to rule out anything more serious before they try to treat their symptoms themselves (or with the help of a pharmacist).
According to NICE guidelines on IBS in adults (updated in April 2017), symptoms may overlap with other gastrointestinal disorders, such as inflammatory bowel disease or coeliac disease, making the condition difficult to diagnose. Anyone with IBS symptoms should consult their GP to rule out anything more serious before they try to treat their symptoms themselves (or with the help of a pharmacist). IBS can’t be ‘cured’, so the aim of treatment is to ease the symptoms and reduce the frequency of flare-ups. Once diagnosed, IBS patients should keep a symptom diary to try to establish their main triggers, assessing their sleeping habits, eating habits, exercise levels and intake of certain foods or drinks (e.g. caffeine, fat, alcohol and/or gas-producing foods such as cabbage).
IBS can’t be ‘cured’, so the aim of treatment is to ease the symptoms and reduce the frequency of flare-ups. Once diagnosed, IBS patients should keep a symptom diary to try to establish their main triggers, assessing their sleeping habits, eating habits, exercise levels and intake of certain foods or drinks (e.g. caffeine, fat, alcohol and/or gas-producing foods such as cabbage).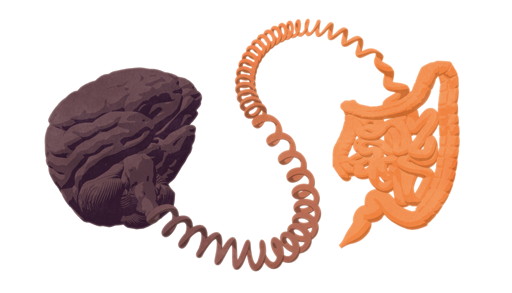 Until recently, IBS was considered to be purely a disorder of bowel function but it is now referred to as a disorder of gut-brain interaction, with the involvement of the gut microbiota/microbiome (altered or unhealthy levels of bacteria in the gut). The gut microbiota is a hot topic of research, and it is hoped that targeting the gut-brain axis will lead to new IBS treatments in the future, particularly for stress-related symptoms.
Until recently, IBS was considered to be purely a disorder of bowel function but it is now referred to as a disorder of gut-brain interaction, with the involvement of the gut microbiota/microbiome (altered or unhealthy levels of bacteria in the gut). The gut microbiota is a hot topic of research, and it is hoped that targeting the gut-brain axis will lead to new IBS treatments in the future, particularly for stress-related symptoms. Mark Cox, consultant gastroenterologist at Spire Little Acton and Spire Parkway Hospitals, says it is important that pharmacists reassure IBS patients about their symptoms once they have been diagnosed. “The initial pharmacy management is usually reassurance that there is nothing sinister going on and that the symptoms are likely to resolve with time,” he says.
Mark Cox, consultant gastroenterologist at Spire Little Acton and Spire Parkway Hospitals, says it is important that pharmacists reassure IBS patients about their symptoms once they have been diagnosed. “The initial pharmacy management is usually reassurance that there is nothing sinister going on and that the symptoms are likely to resolve with time,” he says. Some people find that one specific food triggers their IBS symptoms and, depending on the food, they may be able to cut it out of their diet or at least reduce consumption. NICE guidance stresses, however, that customers planning a restricted diet should seek advice from a dietitian to make sure they are still obtaining enough essential nutrients.
Some people find that one specific food triggers their IBS symptoms and, depending on the food, they may be able to cut it out of their diet or at least reduce consumption. NICE guidance stresses, however, that customers planning a restricted diet should seek advice from a dietitian to make sure they are still obtaining enough essential nutrients. Recent research for Coeliac UK shows diagnoses of coeliac disease rose by a quarter from 24 to 30 per cent between 2011 and 2015 but the rate of diagnosis is now slowing significantly. As a result, around half a million people in the UK are still living with undiagnosed coeliac disease.
Recent research for Coeliac UK shows diagnoses of coeliac disease rose by a quarter from 24 to 30 per cent between 2011 and 2015 but the rate of diagnosis is now slowing significantly. As a result, around half a million people in the UK are still living with undiagnosed coeliac disease.