Clinical

Here comes the sun
In Clinical
Let’s get clinical. Follow the links below to find out more about the latest clinical insight in community pharmacy.Bookmark
Record learning outcomes

Customers should be offered personalised advice on their level of sun exposure to balance their risks of skin damage and vitamin D deficiency
Â
Learning objectives
After reading this feature you should be able to:
- Explain the different roles vitamin D is thought to play in the body
- Discuss dietary sources of vitamin D
- Identify which groups of people require vitamin D supplements.
Â
Exposure to sunlight has been known to be therapeutic for centuries and today UV therapy remains an important treatment for skin conditions such as psoriasis and eczema.
Another valuable action of sunlight on the skin is the production of vitamin D, which has an important role to play in ensuring adequate amounts of calcium and phosphorus are absorbed through the intestine for bone health. In recent years it has become increasingly clear that vitamin D has numerous other roles in the body, as witnessed by the large number of tissues that possess vitamin D receptors.
It is now believed that vitamin D plays an important role in the regulation of cell growth, neuromuscular and immune functions as well as having an anti-inflammatory role. Other research shows that low levels of vitamin D are associated with a range of problems including diabetes, cardiovascular disease, depression, cognitive decline and multiple sclerosis.
Protective role
A possible protective role of vitamin D in cancer has been raised in several observational studies, which found a lower incidence of certain cancers (e.g. colorectal, breast, prostate and pancreatic) among people living in southern latitudes.
Nevertheless, as dermatologist and cancer specialist, Charlotte Proby, says, “only colorectal cancer appears to be associated with vitamin D deficiency and that may be for other – spurious – dietary reasonsâ€. Nonetheless, she believes that vitamin D is definitely important for other conditions including autoimmune diseases and conditions such as multiple sclerosis, as well as for bone health.
While direct evidence of the benefit derived from increasing levels of vitamin D for these conditions is currently unclear, several on-going trials are trying to address the importance of vitamin D in diabetes, respiratory disease and cancer.
Sunshine vitamin
Vitamin D has been termed the ‘sunshine vitamin’ because few foods contain it in sufficient amounts. Up to 90 per cent of vitamin D is obtained from exposure to sunlight. The term ‘vitamin D’ actually refers to two separate compounds: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). The latter is produced by the action of sunlight in plants and is the form of vitamin D obtained from non-animal food sources.
On reaching the skin, UV radiation converts 7-dehydrocholesterol, which is present in cell membranes, into pre-cholecalciferol. This pre-vitamin D is thermally unstable and converts into cholecalciferol, which is then taken up into the circulation. Prolonged exposure to sunlight does not lead to greater production of cholecalciferol and in fact leads to the breakdown of both pre-vitamin D and cholecalciferol.
Cholecalciferol is further metabolised in the liver to 25-hydroxyvitamin D3 (25(OH)D) and then broken down by the kidneys into 1,24-dihydroxyvitamin D3 (calcitriol). This latter compound is the active metabolite, although 25(OH)D is the main circulating form of vitamin D that is measured and provides a reliable assessment of vitamin D stores. Being lipid soluble, cholecalciferol is taken up and stored by adipocyte cells.
According to Leslie Rhodes, professor of experimental dermatology and a member of the NICE advisory group on sunlight and vitamin D, “how long the body stores vitamin D is not completely known but the circulating levels of 25(OH)D fall from a peak at summer end (September) to a trough at winter end (February) in the UKâ€.
The recommended daily allowance (RDA) is the term used to describe the amount of vitamin D required for bone health and calcium metabolism in healthy individuals. For those aged between 19 and 70 years, the RDA is 600 IU (15mcg), rising to 800 IU (20mcg) in the 70+ age group.
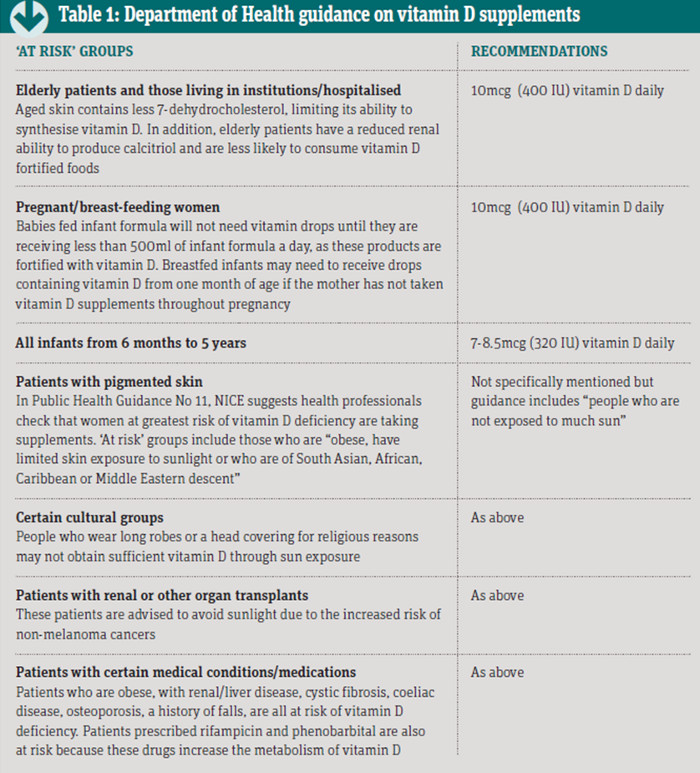
Consequences of vitamin D deficiency Vitamin D deficiency is cited as the commonest nutritional deficiency worldwide although there is a lack of consensus on what constitutes deficiency. In 2012, the Department of Health issued guidance on the groups of patients who should take vitamin D supplements (see Table 1 below), while the Institute of Medicine has defined three threshold levels of vitamin D for optimal bone health:
- Plasma levels of 25(OH)D less than 30nmol/L = vitamin D deficient
- Plasma levels of 25(OH)D 30-50nmol/L = vitamin D inadequate for some people
- Plasma levels of 25(OH)D > 50nmol/L = vitamin D level sufficient for the whole population.
To achieve plasma levels greater than 25nmol/L requires supplementing with 9mcg/day (360 IU) of vitamin D3 during the winter months. Whether the average person should take a vitamin D supplement remains a subject of debate. Professor Rhodes suggests it depends on what circulating levels of 25(OH)D are to be maintained.
“Eating oily fish will assist, as will consuming vitamin D fortified foods,†he says. “Taking a vitamin D supplement of 400 IU will help maintain the vitamin D status of the person in winter.†The most well-known adverse effect of vitamin D deficiency is rickets, a condition affecting bone development in children, leading to soft, weakened bones and bone deformities.
In adults, the condition is called osteomalacia and occurs because of reduced mineralisation in the bone matrix. Evidence suggests that the incidence of rickets is increasing.
Â
Key factsÂ
- Vitamin D is known as the ‘sunshine vitamin’ because few foods contain it in sufficient amounts
- The most well-known adverse effect of vitamin D deficiency is rickets
- Whether the average person should take a vitamin D supplement remains a subject of debate
Â
Treating vitamin D deficiency
Diagnosing vitamin D deficiency is challenging because patients complain of non-specific symptoms such as aches and pains, tiredness and a general sense of malaise. More severe symptoms in children will include soft skull and leg bones, and muscle pains or weakness. Vitamin D deficiency can be corrected through the use of oral cholecalciferol 20mcg (800 IU) daily for up to three months, although higher doses might be needed depending on the severity of the deficiency.
Patients may require maintenance therapy but this depends on their calcium intake. Where calcium intake is low to medium (i.e. less than 500mg/day or between 500mg and 1,000mg/day), then cholecalciferol 800 IU daily and between 500mg and 1,000mg of calcium is required. Where calcium intake is adequate, cholecalciferol 800 IU daily will suffice.
Vitamin D and sunlight
UV radiation induces DNA damage in the skin and it is now considered to be a carcinogen. In addition, because eyelid skin is thin, UV radiation can lead to eye problems such as cataracts. Production of vitamin D (due mainly to UVB radiation) is highest when the sun reaches its peak around noon but this is also the time when most damage is likely to occur to the skin and eyes.
In the UK, exposing the face and arms to the sun for up to 15 minutes, three times a week between March and September, is normally sufficient to produce enough vitamin D. This requirement would need to be increased in those with pigmented skin.
Nevertheless, as Charlotte Proby says, patients should “know their own skin, avoid sunburn or even skin getting red, as this will destroy the vitamin D that has been made, and take vitamin D supplements if they are at risk of being vitamin D deficientâ€.
Sun protection measures
Protecting the skin can be achieved in several ways:
Sunscreen use
Ideally patients should use a product with a SPF of 30 and star rating of 4-5 to get a good, standard of sun protection. Apply sunscreens to dry skin at least 30 minutes before going in the sun and re-apply every two hours – more frequently if the cream is rubbed/washed/sweated off. It should be noted that sunscreens reduce some, but not all, of vitamin D production in the skin.
Clothing
Some clothing manufacturers use the ultraviolet protection factor (UPF). The higher the UPF, the greater the level of protection. Darker fabrics provide more protection than lighter clothes. Also wet clothes only provide about a third of the UV protection, so should be changed if staying in the sun. UV radiation can also damage the eyes so UV protective eyewear is important. Look for the CE mark on the label – this provides protection against UV radiation up to 400nm, which covers the full UV range. A wide-brim hat is also important.
Avoiding the sun at specific times
The greatest risk of burning (due to UVB radiation) occurs when the sun is highest in the sky between 11am and 3pm.
Conclusion
NICE is currently in the process of producing guidance on balancing the risks and benefits of sun exposure but, based on the available evidence, it seems prudent that short bursts of sun exposure around midday before burning, are sufficient for the production of vitamin D. For those who cannot tolerate such exposure, supplementing with vitamin D (preferably vitamin D3) would appear to be a safe and sensible alternative.
